Trying to conceive but not getting answers? You’re not alone — according to the CDC, 1 in 5 married women aged 15–49 in the U.S. struggle with infertility after a year of trying. If you’ve been running in circles with vague diagnoses or “just relax” advice, it’s time to get real answers.
This guide breaks down laparoscopy for infertility—a minimally invasive procedure that helps your doctor see what’s actually going on inside. From diagnosis to recovery, including findings from various meta analysis here’s everything you need to know, minus the medical jargon and fluff.
What Is Laparoscopy for Infertility and Who Needs It?
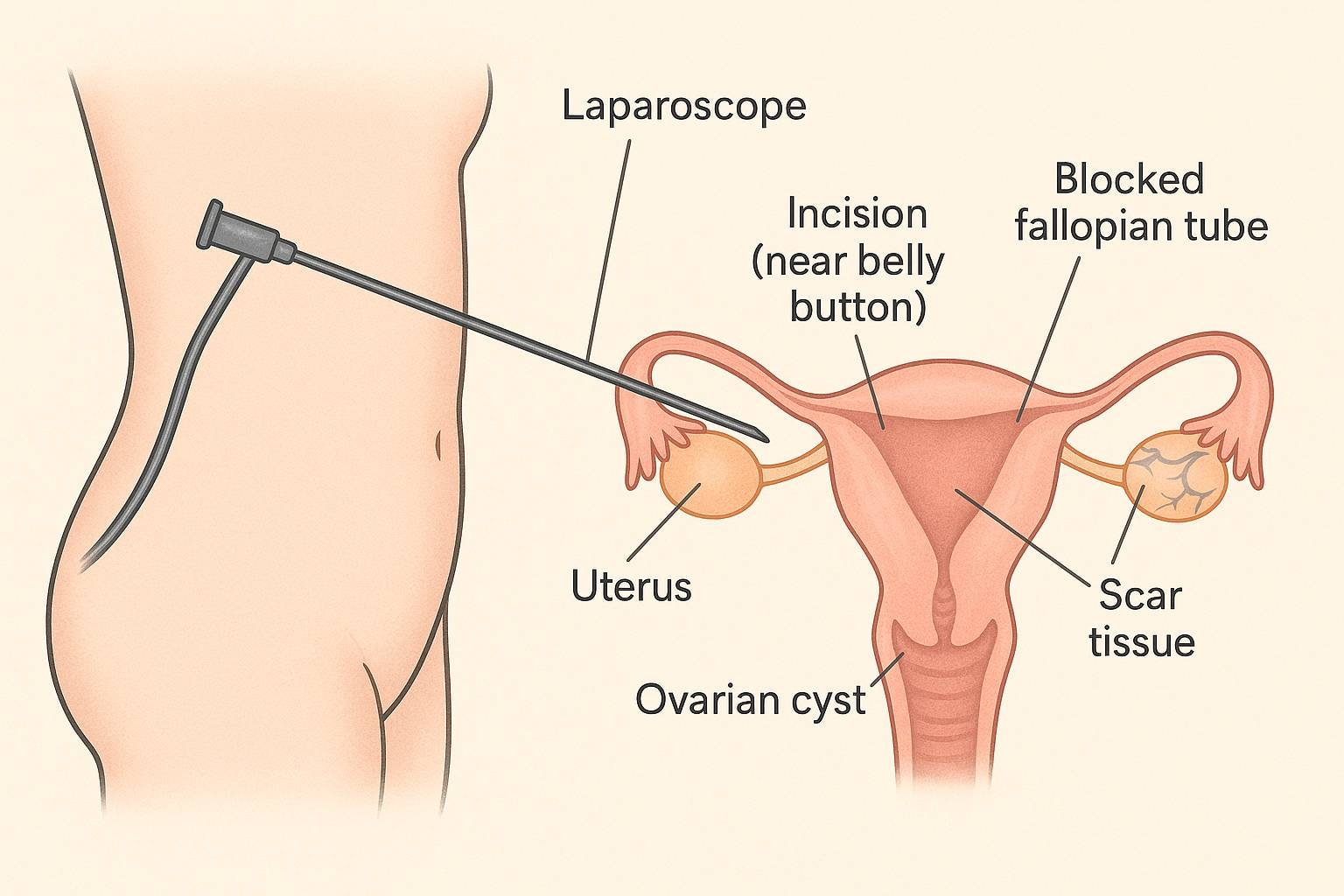
Laparoscopy for infertility is a minimally invasive procedure. It helps your doctor look inside your lower belly using a small camera. This test checks for issues like blocked fallopian tubes, scar tissue, ovarian cysts, or endometriosis lesions—which can affect your ability to get pregnant.
You may need it if:
- Other fertility tests don’t find the problem
- You have pelvic pain or irregular periods
- Your doctor suspects infertility caused by abnormal pelvic anatomy
Laparoscopy is considered one of the most effective methods for diagnosing and treating infertility, especially when other methods fail to identify the cause.
“Laparoscopy is the gold standard for diagnosing endometriosis,” says the American College of Obstetricians and Gynecologists.
It’s safe, helpful, and can improve pregnancy outcomes.
Fertility Tests: The First Step Before Considering Laparoscopy
Before recommending laparoscopy, most fertility specialists begin with non-invasive tests to understand why conception hasn’t happened yet. These fertility tests provide key insights into both male and female reproductive health and help guide the next steps in treatment.
Before laparoscopy, your doctor may repeat certain fertility tests to confirm hormone balance, egg health, and tube function.
- Blood Tests for Hormones: Doctors may check hormone levels such as FSH (Follicle-Stimulating Hormone), LH (Luteinizing Hormone), AMH (Anti-Müllerian Hormone), prolactin, and thyroid hormones. These reveal if ovulation is regular and whether egg reserves are healthy.
- Ultrasound and Follicular Study: A pelvic ultrasound helps visualize the uterus, ovaries, and fallopian tubes. It detects cysts, fibroids, or polycystic ovaries that may affect fertility. Follicular tracking also shows if and when ovulation occurs.
- Hysterosalpingography (HSG): This X-ray-based test checks if the fallopian tubes are open or blocked by injecting a dye through the cervix. It’s a quick way to identify physical barriers that prevent sperm and egg from meeting.
- Semen Analysis for Men: Male fertility tests assess sperm count, shape, and movement. It’s a simple yet crucial step since male factors contribute to about 40–50% of infertility cases.
These tests can sometimes uncover the root cause of infertility—like hormonal imbalance or tubal blockage—without needing surgery. But when the cause remains unclear or requires closer examination, laparoscopy becomes the next best diagnostic option.
When Is Laparoscopic Surgery Recommended for Fertility Issues?
Laparoscopy for infertility is often used when common fertility tests don’t explain why you’re not getting pregnant. Doctors recommend it when they suspect issues inside your belly that can't be seen through ultrasound.
You might need it if:
- You have pelvic pain, scar tissue, or a history of infection
- You may have blocked fallopian tubes, endometriosis lesions, or ovarian cysts
- Your doctor wants to check pelvic anatomy, reproductive organs, or the uterine cavity
“Laparoscopic surgery helps in treating infertility by offering an accurate diagnosis with less pain,” says Dr. Anshu Agrawal, infertility expert.
This minimally invasive procedure gives answers—and sometimes, a solution too.
Step-by-Step: How the Laparoscopy Procedure Works

1. Pre-Procedure Preparation
Before the procedure, you’ll meet your surgeon and medical team. They’ll ask questions about your previous surgeries, health issues, and fertility history.
- You’ll need a few blood tests and maybe an ultrasound to check your uterus and ovaries.
- Your doctor may also check your fertility tests to decide what to look for inside.
- You’ll be given general anesthesia, which means you’ll sleep through the surgery and feel no pain.
- This is often done as an outpatient procedure, so most patients go home the same day.
“Laparoscopy helps us diagnose hidden conditions like endometriosis or tubal blocks that standard imaging can’t show,” says Dr. Anshu Agrawal, infertility specialist.
2. Small Incisions Are Made
Once you’re asleep, the surgeon makes small incisions (cuts) near your belly button and lower abdomen.
- Through one of these incisions, a small camera is inserted to see your reproductive organs, including the fallopian tubes, ovarian cysts, and uterine cavity.
- More instruments may be added through other tiny cuts if treatment is needed. During the procedure, doctors carefully insert instruments through small incisions to examine and treat any underlying issues.
- Since it’s a laparoscopic surgery, the scars are small and healing is faster compared to open surgery.
While rare, there is a risk that abdominal or pelvic organs could be damaged by surgical instruments during the insertion of the camera or other tools.
3. Carbon Dioxide Is Used to Inflate the Abdomen
To see your abdominal organs clearly, doctors pump carbon dioxide gas into your abdominal wall.
- This lifts the organs slightly, giving the surgeon space to work.
- It allows a better view of pelvic anatomy and helps in accurate diagnosis of problems like pelvic pain, endometriosis, or pelvic adhesions.
- After inspection or treatment, the gas is removed and cuts are closed.
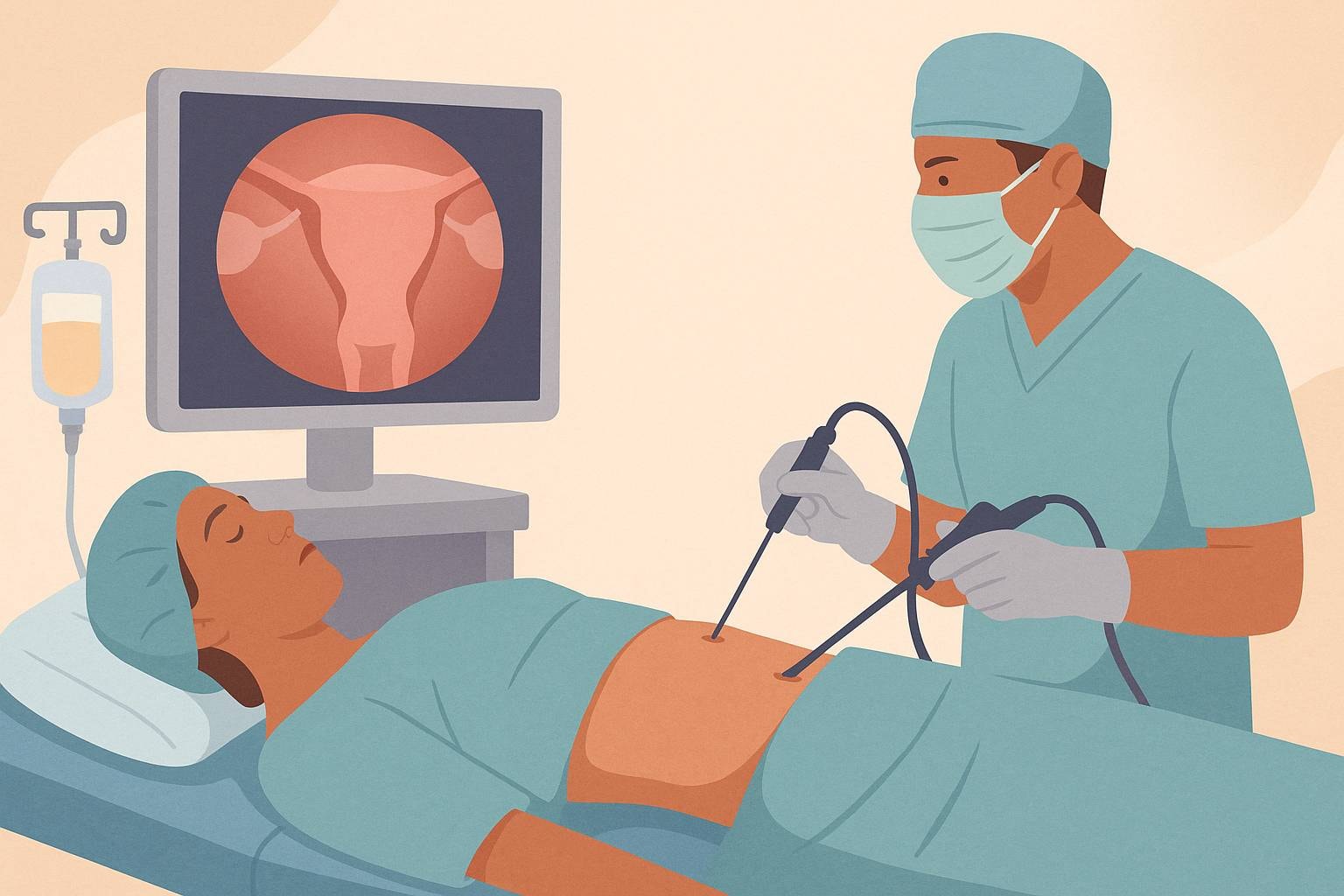
4. Insertion of the Laparoscope
After your belly is filled with carbon dioxide, the surgeon gently inserts a laparoscope—a thin tube with a small camera—through one of the small incisions, usually near the belly button.
- This camera shows real-time images of your reproductive organs like the fallopian tubes, ovaries, uterus, and abdominal organs on a screen.
- It gives a clear look at your pelvic anatomy, helping the doctor find hidden problems that may be affecting your ability to conceive.
- This step is key for making an accurate diagnosis of issues such as scar tissue, endometriosis lesions, or blocked fallopian tubes.
- Sometimes, endometriosis or other abnormalities may be found during laparoscopy, even if previous imaging or tests were negative.
“The laparoscope lets us see more than any scan. It’s precise, fast, and often life-changing,” says Dr. Anshu Agrawal, a fertility surgeon with 20+ years of experience.
5. Inspection and/or Treatment
During the inspection, your doctor may also perform surgical treatment if they spot something that can be fixed right away.
- Common treatments include removing ovarian cysts, cleaning pelvic adhesions, or treating infertility laparoscopy cases involving endometriosis. Studies have shown that treating endometriosis or adhesions during laparoscopy can improve fertility outcomes.
- If your uterine cavity or organs show abnormalities, they might be corrected during the same session.
- This dual purpose—both seeing and treating—is what makes laparoscopy for infertility so valuable.
6. Closing the Incisions
Once the procedure is complete, the gas is gently released, and the small incisions are closed with stitches or surgical glue.
- Since this is a minimally invasive procedure, the cuts are tiny and usually leave little to no scar. However, there is still a small risk of scarring, which could affect reproductive organs.
- Most patients go home the same day and feel less pain compared to traditional surgery.
- Doctors will give you aftercare instructions and schedule a follow-up to review findings and next steps.
7. Post-Procedure Monitoring
After your laparoscopy for infertility, you’ll rest in a recovery room while the effects of general anesthesia wear off.
- Nurses will check your blood pressure, pain levels, and abdominal area.
- You might feel bloated or sore due to leftover carbon dioxide in your abdomen, but this usually goes away in a day or two.
- The small incisions are covered with bandages and need to stay clean to avoid infection.
Most women recover within one to two weeks, but full healing may take several weeks depending on the extent of the procedure.
You’ll be sent home the same day in most cases. Your doctor will tell you:
- When to return for a follow up
- How to care for your surgical wounds
- What symptoms—like fever or heavy bleeding—to watch out for
If your doctor removed ovarian cysts, scar tissue, or treated endometriosis lesions, they’ll explain what was done and what it means for your fertility.
“Recovery is usually smooth, and most women return to work in under a week,” says Dr. Anshu Agrawal, fertility surgeon.
This step closes the loop on your minimally invasive procedure, offering answers and hope in your infertility treatment journey.
What Conditions Can It Diagnose or Treat?
Laparoscopy for infertility helps doctors find and fix problems that may stop you from getting pregnant. It gives a clear view of your reproductive organs, such as the fallopian tubes, uterus, and ovaries.
Here’s what it can find or treat:
- Blocked fallopian tubes that prevent the egg and sperm from meeting
- Endometriosis lesions or endometriosis, where tissue grows outside the uterus
- Ovarian cysts that can affect ovulation
- Pelvic adhesions or scar tissue that stick organs together
- Abnormalities inside the uterine cavity
- Pelvic pain linked to infertility
“Laparoscopy gives us an accurate diagnosis and a chance to treat problems in the same procedure,” says Dr. Anshu Agrawal.
This minimally invasive procedure is often the best way to understand hidden causes of infertility, especially when other fertility tests don’t explain why you're not getting pregnant.
Benefits of Infertility Laparoscopy: More Than Diagnosis

How It Impacts Your Fertility Journey
Laparoscopy for infertility is not just for finding problems. It also helps fix them. Here’s why it works well:
- Diagnose and Treat in One Go: Laparoscopy doesn’t just look for problems—it can fix them on the spot. Doctors can remove ovarian cysts, scar tissue, or endometriosis lesions during the same procedure.
- Improves Natural Conception Chances: By restoring normal pelvic anatomy, laparoscopy can unblock fallopian tubes or treat pelvic adhesions, making it easier for the egg and sperm to meet.
- Minimally Invasive, Faster Recovery: It’s a minimally invasive procedure, meaning smaller cuts, less pain, and quicker healing compared to open surgery. Most patients go home the same day.
- Accurate Diagnosis When Other Tests Fail: If ultrasounds and scans don’t show the cause of infertility, laparoscopy gives a clear view of your uterus, fallopian tubes, and abdominal organs, helping doctors make an accurate diagnosis.
- Reduces Need for Multiple Procedures: Since laparoscopic surgery can treat many issues in one session, it reduces the need for repeat procedures and lowers overall medical costs and stress.
- Better Understanding of Hidden Conditions: It helps detect severe endometriosis, blocked fallopian tubes, and pelvic pain causes that are hard to see with regular imaging.
It also increases your chances of natural conception by restoring normal pelvic anatomy. This is especially helpful if you have endometriosis lesions, infertility laparoscopy cases, or pelvic pain that’s been hard to explain.
Current research suggests laparoscopic intervention can significantly increase the chances of natural conception in selected patients.
Is Laparoscopy Safe? What Risks Should You Know?
Laparoscopy for infertility is a minimally invasive procedure that helps doctors see inside your abdomen and treat problems like blocked fallopian tubes, endometriosis, or scar tissue.
It’s often called keyhole surgery because it uses small incisions to avoid big cuts. This makes it less painful and helps you heal faster. But like any surgical treatment, it has some risks.
What Are the Possible Risks?
While laparoscopy for infertility is considered generally safe, some risks include:
- Infection at the site of small incisions
- Injury to abdominal organs, blood vessels, or other organs
- Problems from general anesthesia
- Pelvic adhesions may form after surgery, though less common
- Mild pelvic pain or bloating from carbon dioxide used during the procedure
One study from the Journal of Reproductive Medicine noted that fewer than 2 in 100 women had serious issues. That means 98% of women recovered well with no major problems.
Recovery and What to Expect After Surgery
Recovering after a laparoscopy for infertility is usually smooth. It’s a minimally invasive procedure, so healing time is often faster than open surgery. But your body still needs care.
Here’s what you can expect:
1. First Few Hours After Surgery
- You may feel sleepy or groggy due to general anesthesia.
- Some women feel pain near the belly button or in the shoulder due to carbon dioxide used to inflate the abdomen during surgery.
- Doctors check for bleeding or problems before sending you home.
2. First Few Days
- Mild pelvic pain, bloating, or soreness is common.
- You may notice bruising near the small incisions.
- Avoid heavy lifting or bending.
3. One Week Later
- Most women return to work in 5–7 days.
- If surgical treatment was done for ovarian cysts, scar tissue, or endometriosis lesions, full recovery may take longer.
- A follow-up visit ensures healing and reviews fertility treatment options.
“Laparoscopy allows many women to resume daily activities within a week,” says the American College of Obstetricians and Gynecologists.
Tips for Faster Recovery:
- Eat light, easy-to-digest meals.
- Keep the incision area clean and dry.
- Rest when tired — don’t rush back too soon.
Dr. Anshu Agrawal’s Expertise in Treating Infertility Laparoscopy

Dr. Anshu Agrawal is one of Ranchi’s most trusted specialists for laparoscopy in infertility. With 18+ years of clinical experience, she focuses on diagnosing and treating root causes of infertility through advanced, minimally invasive procedures.
Her hands-on expertise is backed by modern equipment, strong surgical outcomes, and a deeply personalized approach to patient care.
Here’s why patients across Jharkhand and beyond choose her for infertility laparoscopy:
- Over 1,200+ successful infertility surgeries: Her clinic has performed 1,200+ laparoscopic and hysteroscopic procedures — many of which helped women conceive naturally without IVF. That’s not just experience; that’s proven outcomes.
- Special focus on blocked fallopian tubes & endometriosis: She uses laparoscopy to accurately diagnose and treat issues like scar tissue, ovarian cysts, and endometriosis lesions — key factors that often go undetected in basic fertility tests.
- Reduces surgical pain, downtime, and costs: With keyhole surgery techniques, most patients are discharged within 24–48 hours. Faster recovery means fewer complications, less time off work, and lower emotional stress.
- Combines treatment with empathy: Dr. Agrawal is known for her calm, friendly consultations. Patients often say they feel heard and understood — not rushed or pressured into expensive options.
- Trained at top institutes, backed by research: MBBS from Eras Lucknow Medical College. MS in Obs-Gyn from Motilal Nehru Medical College. She regularly contributes to OB-GYN journals and keeps her protocols updated with the latest in reproductive medicine.
“Laparoscopy isn’t just about diagnosis. It’s about restoring confidence, health, and the chance to conceive — naturally if possible.” — Dr. Anshu Agrawal
📍 Clinic Address: Dr. Anshu Agrawal’s Clinic
Opposite Ranchi Women’s College, Circular Road, Ranchi, Jharkhand – 834001
🌐 Website: www.dranshuagarwal.com
🕒 Clinic Hours: Monday to Saturday – 10:00 AM to 6:00 PM
Sunday – Closed
If you’re struggling with unexplained infertility, Dr. Agrawal’s laparoscopic approach may help you skip IVF altogether by first fixing the core issues affecting fertility.
Comparing Laparoscopy to Other Infertility Treatments
While laparoscopy for infertility helps diagnose and treat physical problems inside your body, other treatments work differently. Let’s look at some common ones and how they compare.
1. Fertility Medications
Fertility medications are often the first step.
- They help your body release eggs.
- Doctors often suggest these if your fallopian tubes are clear and your partner’s sperm is healthy.
- These medicines can help improve pregnancy outcomes.
But they don’t fix physical issues like blocked fallopian tubes, endometrial tissue, or pelvic adhesions. That’s where laparoscopy has an edge.
“In many cases, fertility medications alone are not enough if the pelvic anatomy is affected,” says the American College of Obstetricians and Gynecologists.
2. Intrauterine Insemination (IUI)
In IUI, sperm is placed directly into the uterine cavity.
- It works best when the problem is mild sperm issues or unexplained infertility.
- It’s less invasive and cheaper than laparoscopy.
- But IUI doesn’t treat causes like tubal patency problems or scar tissue.
Laparoscopic surgery can fix those issues and boost your chance of natural conception later.
3. In Vitro Fertilization (IVF)
IVF means joining egg and sperm outside the body.
- It bypasses blocked fallopian tubes, endometriosis lesions, or abnormalities in the reproductive system.
- It’s powerful but expensive.
- IVF doesn’t treat the root problem — just skips over it.
Laparoscopy can help restore normal pelvic anatomy, improving the success of IVF if needed later.
One study showed that laparoscopy before IVF improved clinical pregnancy rates by up to 30%.
4. Surgical Treatment (Non-Laparoscopic)
Some surgeries are done without laparoscopy.
- These involve large cuts in the abdominal wall.
- They may treat emergency surgery needs or complex problems in the pelvic cavity.
- But recovery is longer, and there’s a higher infection risk.
Operative laparoscopy uses small incisions and a small camera to treat conditions with less pain and faster healing.
Conclusion
Laparoscopy for infertility is not just one method—it’s often called the gold standard. It helps doctors see the reproductive organs, fallopian tubes, and uterine cavity clearly. This means a more accurate diagnosis and better pregnancy outcomes.
If other fertility treatments haven’t worked, this minimally invasive procedure could help. It lowers the increased risk of missed problems like endometriotic lesions or scar tissue.
As Dr. Anshu Agrawal explains,
“Laparoscopy allows us to treat the root cause—so couples have a real shot at natural conception.”
Talk to your doctor. It might be the step you need toward getting pregnant.

.jpg)
.jpg)

.jpg)


