“What now?”
That’s the question many couples ask when nothing else is working. If you’ve landed here, chances are IVF is on your mind—and with it, a mix of hope, fear, and a thousand unknowns.
In vitro fertilization treatment isn’t just a medical process—it’s an emotional journey. Before you dive into appointments and procedures, you need real answers, not just medical terms.
This article gives you exactly that—clear, simple guidance on how IVF works, what to expect, and how to know if it’s the right path for you. No fluff, no confusion—just straight-up help to move forward with confidence.
What is Assisted Reproductive Technology and In Vitro Fertilization?
When natural conception isn’t happening, many people turn to medical help. Assisted Reproductive Technology (ART) is the group of medical methods that help people get pregnant, and in vitro fertilization (IVF) is one of the most widely used types.
How In Vitro Fertilization (IVF) Fits into ART
IVF is a form of infertility treatment that involves combining eggs and sperm outside the body, in a lab. It’s usually suggested when other options haven’t worked, or when there are known fertility problems in one or both partners. A fertility specialist usually oversees the process to guide you step by step.
Before starting IVF, there are important checks. These include blood tests to understand hormone levels and overall reproductive health. The doctor may also perform scans to check the uterus and ovaries. These early steps help decide the best treatment plan.
Once the plan is ready, you’ll likely begin fertility medicines. These drugs help the body produce more eggs than usual so doctors have more chances to create a healthy embryo. The medicines are taken through daily injections or pills over several days.
Some key points to know:
- The IVF cycle involves monitoring, egg collection, fertilization, and embryo transfer.
- It often takes more than one cycle for success.
- Regular blood tests are done throughout to check how your body is responding to the fertility medicines.
Though IVF is safe for most people, it’s important to talk about risks. For example, overstimulation of the ovaries can lead to health issues.
And in rare cases, some studies have looked at links between certain fertility medicines and long-term health risks, like ovarian cancer, though this is still being researched.
In short, IVF is a key part of ART that gives many families a real chance at having a baby. It’s complex, but with the right support and a clear plan, it’s manageable—and hopeful.
What Factors Affect In Vitro Fertilization Success Rate?
IVF success depends on a mix of medical, biological, and lifestyle factors. While some are outside your control, many can be managed with the right care and planning. Understanding these factors helps you ask better questions, set realistic expectations, and prepare wisely.
1. Embryo Health and Development Stage
A high-quality embryo is the single biggest predictor of IVF success. But not every fertilized egg becomes a strong embryo.
- Embryos that reach the blastocyst stage (day 5 or 6) have a higher chance of successful implantation than day 3 embryos.
- Preimplantation Genetic Testing (PGT-A) can identify embryos with the correct number of chromosomes, which improves live birth rates and reduces miscarriage risk.
- Embryos with poor structure, slow development, or chromosomal issues often fail to implant — even if transferred.
Key Tip: Ask your clinic how they grade embryos and what percentage typically reach blastocyst stage in their lab.
2. Egg Quality and Ovarian Reserve
Egg quality declines naturally with age, and it affects everything from fertilization to embryo strength.
- Ovarian reserve refers to how many eggs you have left and how well they respond to stimulation.
- Blood tests like AMH (Anti-Müllerian Hormone) and FSH (Follicle Stimulating Hormone) help assess your reserve.
- Even with many eggs retrieved, poor egg quality can lower your chances of a healthy embryo.
For women with low reserve or poor response, options include mild stimulation, early retrieval, or using an egg donor.
3. Sperm Quality and Fertilization Technique
Healthy sperm matter just as much as healthy eggs.
- Problems like low count, weak movement (motility), or abnormal shape reduce natural fertilization chances.
- In cases of male factor infertility, ICSI (Intracytoplasmic Sperm Injection) is used to inject a single sperm directly into the egg.
- DNA fragmentation in sperm can also affect embryo quality, even if sperm look normal under a microscope.
Tip: Men should also follow fertility-friendly habits: no smoking, reduce heat exposure, stay active, and manage stress.
4. Uterine Health and Lining Thickness
The uterus needs to be ready to accept the embryo. If the uterine lining is too thin, inflamed, or scarred, implantation may fail.
- A lining thickness of at least 7–8mm is generally considered ideal for embryo transfer.
- Conditions like fibroids, polyps, or endometritis can reduce the chances of implantation or increase miscarriage risk.
- An HSG or hysteroscopy may be needed to check the uterus before starting treatment.
Some clinics use estrogen priming, PRP (platelet-rich plasma), or scratch techniques to improve the uterine environment before transfer.
5. Age of the Woman
Age affects both egg quantity and quality. It’s one of the strongest predictors of IVF success.
- Women under 35 have average success rates of 40–50% per IVF cycle, while women over 42 often see rates below 10%.
- Egg freezing at a younger age helps preserve fertility and improve later success.
- Older patients may benefit from PGT, donor eggs, or personalized hormone protocols.
Note: Age also affects miscarriage risk, response to medications, and risk of genetic conditions.
6. IVF Clinic Quality and Lab Conditions
Where you go for treatment makes a difference. Not all clinics use the same equipment, techniques, or protocols.
- A skilled embryologist and a clean, well-controlled lab environment directly affect embryo growth.
- Ask about success rates by age group, use of time-lapse monitoring, and lab grading systems.
- A good lab will also have a strong policy for embryo freezing, thawing, and storage.
Some clinics have higher cumulative success rates across multiple cycles because of stronger lab practices.
7. Number of IVF Cycles Completed
One cycle doesn’t always lead to success. Most patients need 2–3 cycles to achieve a live birth.
- Cumulative success rate increases with each cycle — especially if frozen embryos are available.
- Many couples conceive on their second or third cycle once protocols are adjusted.
- Learning from failed cycles (e.g., changing stimulation meds, timing, or using PGT) often improves outcomes.
Pro Tip: Don’t see a failed cycle as wasted—it gives valuable data that can improve the next round.
8. Type and Timing of Embryo Transfer
Fresh vs. frozen transfer can make a difference, depending on your hormone levels and uterine health.
- Frozen embryo transfers (FET) are sometimes more successful because the body isn’t recovering from stimulation drugs.
- Single embryo transfer (SET) lowers the risk of multiple births, which carry more complications.
- Timing is crucial — the embryo must sync with the uterine lining (known as the "implantation window").
Some clinics use ERA (Endometrial Receptivity Analysis) to find the ideal transfer day for your body.
Final Thought
No one factor determines IVF success — it’s always a combination. But understanding the full picture helps you ask better questions, work closely with your doctor, and make informed choices along the way.
Curious how these factors apply to your case? Book a one-on-one consult at Dr. Anshu Agarwal’s Clinic and get answers tailored to your story.
Differences Between IVF Process, IUI process, and Other ART Methods
There’s more than one way to treat infertility, and not all methods work the same. Here’s a quick look at how IVF, IUI, and other common ART options compare.
Each method has its own use case depending on the cause of infertility and the advice from your fertility specialist. Knowing the differences helps you choose the right infertility treatment path with confidence.
How Fallopian Tube Damage and Other Factors Cause Infertility
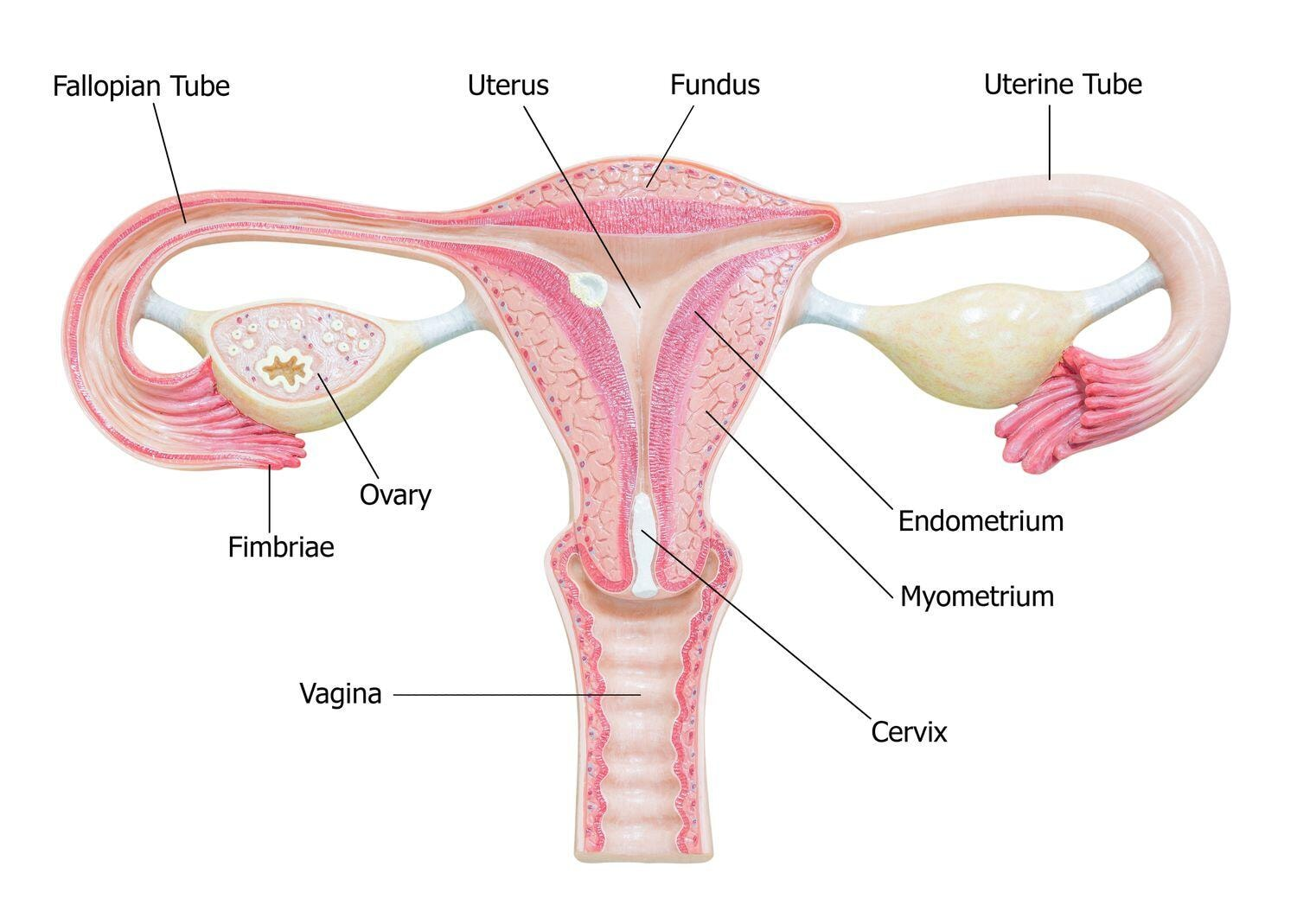
For pregnancy to happen naturally, several parts of the reproductive system need to work together. If even one part is blocked or damaged, it can lead to infertility. One of the most common causes is damage to the fallopian tubes.
Fallopian tubes carry the egg from the ovary to the uterus. If they are blocked or scarred, the egg and sperm can’t meet. This can happen due to infections, past surgeries, or conditions like endometriosis.
Other factors that may cause infertility include:
- Hormonal imbalances that affect ovulation
- Low sperm count or poor sperm movement
- Age, which reduces egg quality and number
- Uterine fibroids or other structural problems
- Lifestyle factors like smoking, poor diet, or high stress
In many cases, these issues are found through blood tests, ultrasounds, or exams done by a fertility specialist. Once the cause is clear, the right infertility treatment—like IVF or IUI—can be planned to improve the chances of pregnancy.
Still feeling unsure? Ask your biggest question —sometimes, clarity starts with just one honest conversation
IVF Treatment Step-by-Step: Egg Retrieval, ICSI, Embryo Culture, and Embryo Transfer
IVF is a type of reproductive medicine that uses several steps to help people who can’t conceive naturally. Each step is designed to prepare the eggs and sperm, promote fertilization, and give the embryo the best chance to develop and lead to a live birth.
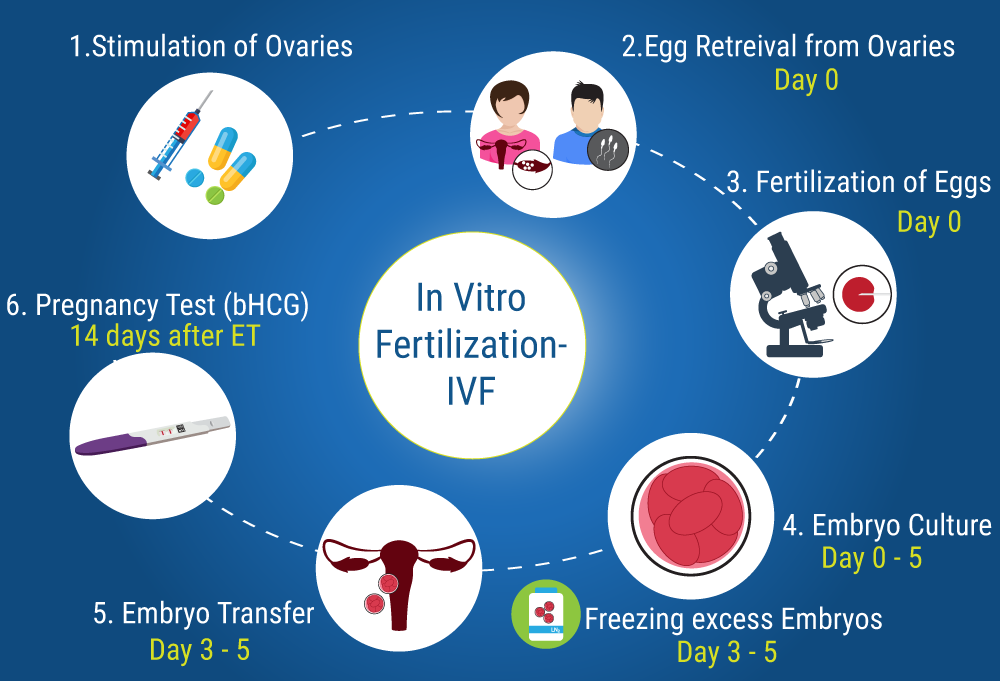
1. Ovarian Stimulation Using Fertility Drugs
The IVF journey starts with fertility medications to increase egg production. These drugs, often containing follicle stimulating hormone, help the ovaries produce several eggs instead of one. More eggs mean more chances to create healthy embryos.
- This step is also called inducing ovulation.
- Regular scans and blood tests check hormone levels and ovarian follicles.
- Your fertility clinic may also do ovarian reserve testing at this stage to see how your body will respond.
Additional Info:
Some women respond quickly, while others may need more days of stimulation. Close monitoring is key to avoid overstimulation, known as OHSS. Clinics may adjust doses based on how your body reacts.
2. Final Maturation Trigger and Timing
When the eggs are ready, an injection of human chorionic gonadotropin is given to help each mature egg reach its final stage. Correct timing is critical to make sure the eggs are at their best stage for retrieval.
- This step also prepares the uterine lining for the embryo.
- Doctors watch carefully so you don’t end up with more than one embryo developing naturally, which could lead to multiple births.
Additional Info:
Timing mistakes at this stage can affect egg quality. The egg retrieval must happen about 36 hours after the trigger shot to catch the eggs before ovulation.
3. Egg Retrieval Procedure
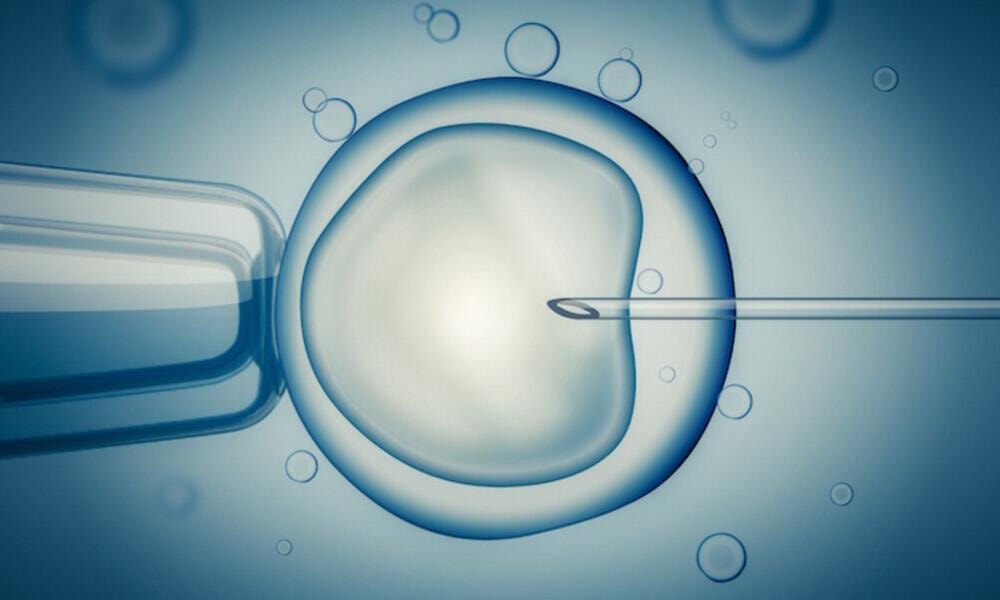
About 34–36 hours after the trigger, the eggs are removed in a process called egg retrieval. This involves a transvaginal ultrasound aspiration done under light sedation. Doctors collect the eggs from the ovaries in a short procedure.
- This process is also called oocyte retrieval.
- The clinic may use eggs from you or an egg donor depending on the case.
- At this stage, infectious disease screening is also done to ensure safety.
Additional Info:
Recovery is usually quick, but mild cramping or spotting is common. The number of mature eggs retrieved often depends on age and ovarian reserve.
4. Semen Collection and Sperm Preparation
The partner provides a semen sample on the same day. If needed, donor sperm may be used. The lab team then washes and prepares the sperm to remove sperm abnormalities and pick the best ones to fertilize the eggs.
- This step increases the chance to achieve pregnancy.
- It is also part of other assisted reproductive technology like artificial insemination.
Additional Info:
Sperm preparation techniques include density gradient washing or swim-up methods to isolate motile sperm. For men with severe sperm issues, surgical retrieval may be used.
5. Fertilization via Conventional IVF or Intracytoplasmic Sperm Injection (ICSI)
Once the eggs and sperm are ready, fertilization is done. This can happen either through conventional vitro fertilisation or by directly injecting one sperm into each egg (ICSI).
- This process creates a fertilized egg (also called a fertilised egg).
- It’s used when there is male factor infertility or previous failed cycles.
- ICSI can help when using own eggs or donor eggs.
Additional Info:
ICSI has become common even in non-male factor cases because it improves fertilization rates. Still, the clinic will decide based on sperm quality and egg count.
6. Embryo Culture and Monitoring
After fertilization, the embryos are kept in a special lab for embryo culture. Here, experts monitor embryo development daily to check embryo status.
- In some cases, embryo hatch or assisted hatching may be used to help the embryo break out of its shell before transfer.
- This period also allows time for embryo storage if needed for later cycles.
Additional Info:
Embryos are typically graded based on appearance and development speed. Clinics may culture embryos to day 3 (cleavage stage) or day 5/6 (blastocyst stage), depending on quality and quantity.
7. Embryo Selection and Optional Genetic Testing
At this stage, doctors pick the healthiest embryos. Preimplantation genetic screening may be done to test for genetic conditions before transfer.
- This can reduce risks for advanced maternal age patients.
- It also helps lower the chances of multifetal pregnancy reduction later.
- Only the embryos with the best chance of a successful pregnancy and good pregnancy rates are selected.
Additional Info:
Testing may include PGT-A (for chromosome screening) or PGT-M (for inherited disease). While optional, it’s often recommended for older patients or those with a history of miscarriage.
8. Embryo Transfer into the Uterus
The chosen embryo is placed into the uterus in a simple, painless step. Sometimes a single embryo is used to increase the chances of singleton pregnancies and avoid multiple embryos being transferred.
- The doctor makes sure the uterine lining is ready for when the fertilized egg attaches.
- This step is often done within a single IVF cycle.
Additional Info:
Embryo transfer is guided by ultrasound to place the embryo in the optimal spot. No sedation is needed, and the procedure takes just a few minutes.
9. Luteal Phase Support and Post-Transfer Care
After transfer, you may be given the hormone progesterone to support the lining of the uterus. This helps the fertilized egg implant properly and maintain early pregnancy.
- Good care at this stage can improve IVF success rates.
- Avoiding negative lifestyle factors also matters for a successful pregnancy.
Additional Info:
Support can come in the form of pills, injections, or vaginal suppositories. Doctors may also monitor progesterone levels and adjust doses if needed.
10. The Two-Week Wait and Pregnancy Testing
Finally comes the wait. Around 10–14 days after transfer, blood tests confirm if implantation has happened.
- Some people achieve pregnancy on the first try; for others, a single IVF cycle varies in results.
- Even if the first attempt fails, there are often more embryos in embryo storage for future use.
Additional Info:
Avoid testing too early with home kits, as medications can give false positives. Clinics rely on beta hCG blood tests to confirm pregnancy accurately.
This step-by-step plan of an IVF cycle helps you clearly see how modern fertility treatments work. By knowing each part, you can prepare better and increase your chances of a healthy, live birth. Working closely with your clinic and following their guidance at each stage makes all the difference.
Intracytoplasmic Sperm Injection (ICSI): A Closer Look at This IVF Technique
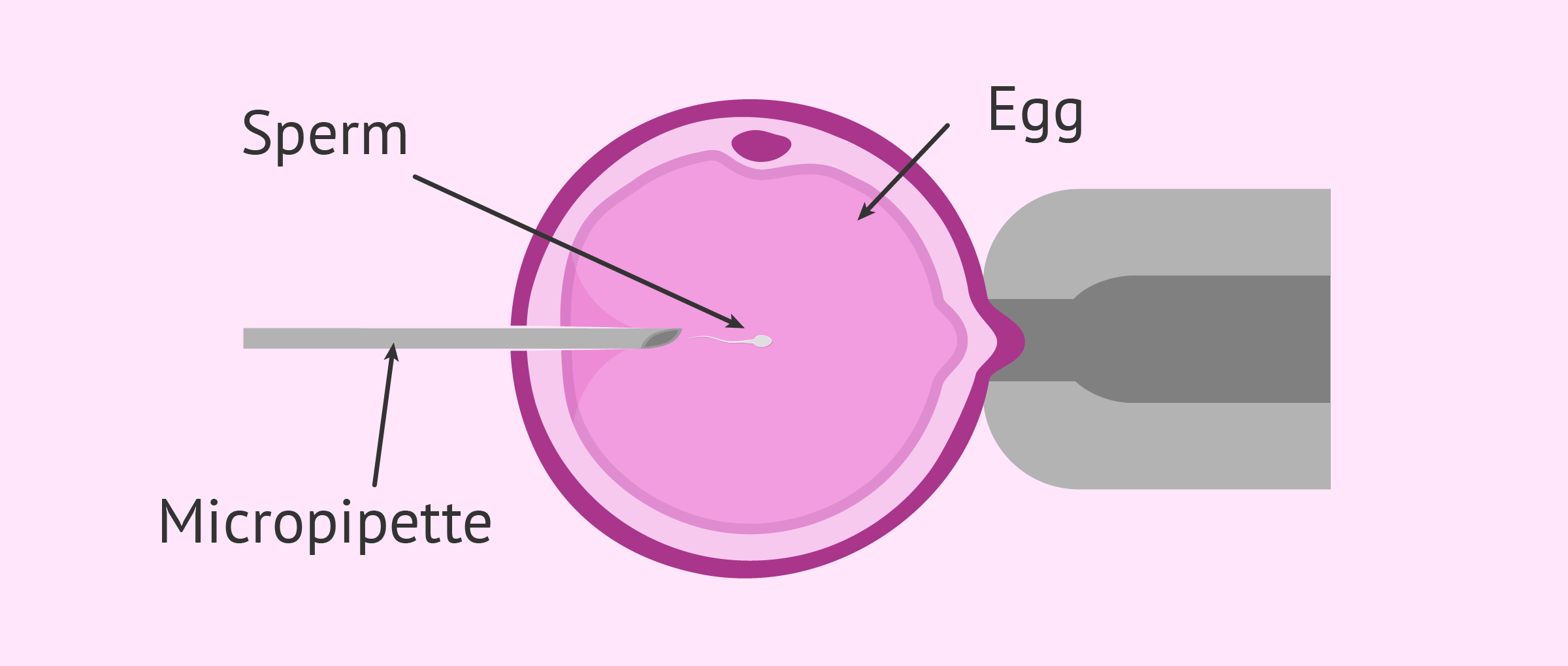
Intracytoplasmic Sperm Injection (ICSI) is an advanced form of vitro fertilisation used as part of an IVF cycle. In ICSI, a single healthy sperm is directly injected into a mature egg to help promote fertilization. This technique is especially useful when sperm quality is poor or there are very few sperm available.
When Is ICSI Recommended?
ICSI is often advised when:
- There are sperm abnormalities (low count, poor movement, or shape issues)
- Previous IVF attempts failed to achieve pregnancy
- There is male factor infertility
- Fertilization needs to be done using frozen sperm, donor sperm, or surgically retrieved sperm
- The couple is using egg donor eggs or performing preimplantation genetic screening
It may also be used in cases where only a few eggs were collected during oocyte retrieval, and each one is valuable.
How Does ICSI Work?
ICSI happens after egg retrieval, during the lab stage of the IVF cycle:
- A single sperm is selected under a microscope.
- This sperm is injected into the mature egg using a fine needle.
- The fertilized egg is then monitored for normal embryo development.
- If development goes well, the embryo is transferred into the uterus.
This process can be paired with embryo storage for future cycles, especially if more than one fertilized egg forms and is viable.
Advantages of ICSI
- Can overcome severe male factor infertility
- Increases pregnancy rates in cases where natural fertilization is unlikely
- Can be used with donor sperm or surgically retrieved sperm
- Helps couples who didn’t conceive naturally despite other fertility treatments
Risks and Considerations
While ICSI is safe for most, it doesn’t guarantee a successful pregnancy. There are also a few risks:
- Egg damage during injection
- Fertilization failure even after ICSI
- Extra cost in a single IVF cycle
If pregnancy occurs, your doctor will closely monitor for any health issues, including gestational diabetes, which is more common in pregnancies achieved through IVF—especially when factors like advanced maternal age or multiple births are involved.
Understanding IVF Costs: What to Expect and Budget For

IVF treatment can be expensive, and the final cost often depends on your clinic, location, and medical needs. Knowing what you're paying for helps you plan better and avoid surprises later.
Here’s what the cost usually includes:
- Initial consultation and fertility testing (blood tests, ultrasounds, semen analysis)
- Fertility medicines for stimulating egg production
- Ultrasound scans and blood tests during the cycle
- Egg retrieval and lab procedures, including ICSI if needed
- Embryo culture and transfer, and sometimes embryo freezing
Extra costs may come from:
- Preimplantation genetic testing (PGT)
- Using donor sperm or donor eggs
- Additional IVF cycles if the first one fails
- Embryo storage fees for frozen embryos
Some clinics offer package plans or EMI options, which can lower the pressure of paying all at once. Always ask for a full cost breakdown before starting treatment.
Planning ahead helps reduce stress and lets you focus on what really matters—getting the right care and giving yourself the best chance to succeed.
Getting ready for IVF isn't just about medical tests. Taking care of your body and mind before starting treatment can improve your results and help you feel more in control.
Steps to Prepare Your Body and Mind for IVF Treatment
Follow these steps to prepare your mind and body for IVF process.
1. Start by focusing on your physical health:
- Eat a balanced diet with plenty of fruits, vegetables, whole grains, and protein. Nutrients like folic acid, vitamin D, iron, and omega-3s are especially important for fertility.
- Maintain a healthy weight — even a small weight loss (5–10%) can help regulate ovulation and improve how your body responds to fertility medications.
- Avoid smoking, alcohol, and exposure to harmful chemicals or toxins. These can reduce egg quality and lower IVF success rates.
Tip: Ask your fertility specialist if you need prenatal vitamins or specific supplements before starting your IVF cycle.
2. Exercise regularly, but not too hard:
- Choose gentle activities like walking, yoga, swimming, or stretching.
- Avoid intense workouts or long cardio sessions, which may impact hormone levels or menstrual cycles.
- Staying active supports blood flow to reproductive organs and helps manage stress.
3. Don't ignore your mental health. IVF can be stressful and emotional:
- Talk to your partner, a therapist, or join a local or online support group to feel less alone.
- Practice simple relaxation techniques like deep breathing, journaling, or guided meditation.
- Stick to a regular routine that includes 7–8 hours of sleep and time for rest and self-care.
Tip: Some clinics offer counseling or mind-body programs to help patients prepare mentally and emotionally for treatment.
Final Thought
Small, consistent changes made before IVF can make a big difference during the journey. You’ll feel stronger, calmer, and more ready—both inside and out—to face each step with clarity and confidence.
Risks of In Vitro Fertilization: Birth Defects, Complications, and Failures

IVF gives hope—but it also brings risks that every couple should know. While many go on to have healthy pregnancies, it’s important to understand what can go wrong before starting treatment. These risks don’t affect everyone, but knowing them helps you make smart, informed choices.
1. Increased Risk of Birth Defects
Some studies suggest a slightly higher chance of birth defects in babies born through IVF. This can be due to the treatment itself or the underlying infertility problems.
- Heart and digestive issues are among the most reported.
- Risk may be higher in advanced maternal age or when fertility treatments are combined.
- Doctors often recommend preimplantation genetic screening to check embryo health before transfer.
- It's also important to manage maternal health and avoid harmful lifestyle factors that could increase the risks.
2. Higher Chance of Multiple Pregnancies
IVF sometimes leads to multiple births, especially when more than one embryo is transferred.
- This can raise the chance of singleton pregnancies turning into twins or triplets.
- Multiple babies increase the risk of early labor and health problems for both mother and babies.
- Some clinics suggest single embryo transfer to lower this risk.
- Multiple pregnancies may also increase the chance of needing cesarean delivery or neonatal ICU support.
3. Premature Birth and Low Birth Weight
Babies born through IVF are more likely to arrive early or have a low weight at birth.
- Multiple embryos in the womb is a big reason for this.
- Early babies may need extra medical care after delivery.
- Even in singleton pregnancies, some risk remains.
- Careful embryo selection and improved lab culture conditions can help reduce this risk.
4. Ovarian Hyperstimulation Syndrome (OHSS)
OHSS happens when fertility medications overstimulate the ovaries. It can cause pain, swelling, and other health issues.
- In rare cases, it leads to fluid buildup and blood clots.
- The risk is higher in younger women with high ovarian reserve testing results.
- Doctors adjust fertility medicines to prevent or control OHSS during treatment.
- Triggering ovulation with lower-dose medications or using GnRH agonists may help lower the risk.
5. Failed Embryo Implantation
Not every fertilized egg attaches to the uterine lining. Implantation failure can happen even if the embryo looks healthy.
- Poor embryo status, uterine lining, or hormonal imbalance may cause it.
- It’s one of the top reasons a single IVF cycle may not lead to pregnancy.
- Testing and adjusting transfer timing may help in future attempts.
- Endometrial receptivity analysis or uterine imaging may help spot unseen problems.
6. Ectopic Pregnancy
This is when the fertilized egg implants outside the uterus, often in the fallopian tube.
- It’s painful and dangerous if not treated quickly.
- IVF doesn’t remove this risk entirely, especially if the woman has past fallopian tube damage.
- Close monitoring after transfer is important to catch it early.
- Symptoms like abdominal pain or unusual bleeding should be reported immediately.
7. Emotional and Financial Stress
IVF can take a toll on mental health and relationships. The wait, failures, or side effects can be emotionally draining.
- Each IVF cycle can also be expensive, especially if insurance doesn’t cover it.
- Not knowing if it will lead to a live birth adds pressure.
- Many clinics offer counseling or support groups to help.
- Emotional support and stress reduction may also improve physical outcomes during the cycle.
8. Risks Associated with Donor Eggs
Using an egg donor can help when a woman’s own eggs aren’t viable, but it comes with its own risks.
- There may be legal, emotional, or ethical concerns.
- Some studies link donor eggs to a slightly higher chance of pregnancy complications.
- Full infectious disease screening of the donor is always done to ensure safety.
- Patients should also be informed about long-term implications for child identity and family planning.
9. Miscarriage After IVF
Even after a positive test, miscarriage can still happen, especially in older women or those with health conditions.
- Hormone support is often used to strengthen the early pregnancy.
- Poor embryo development or genetic issues may be to blame.
- Repeated losses might require extra tests or other assisted reproductive technology options.
- A thorough review of previous cycle data can help tailor the next treatment plan.
10. Long-Term Health Uncertainties for IVF-Conceived Children
Most children born through IVF grow up healthy, but some long-term effects are still being studied.
- Some research is looking at small risks for issues like gestational diabetes in the mother or developmental delays in the child.
- There’s no solid proof yet, but doctors continue to watch for patterns over time.
- Staying in touch with a pediatrician who knows about IVF can help spot any issues early.
- Ongoing health tracking from birth through childhood helps researchers improve future IVF safety.
How to Improve IVF Outcomes and Minimize Birth Defects

IVF results can vary widely, but certain steps are proven to improve your chances of success. From lifestyle choices to lab technology, every decision counts. Here’s how to make your IVF journey safer and more effective.
1. Optimize Maternal Age
Age affects both the quantity and quality of eggs. The younger you are, the higher your chances of producing healthy embryos that lead to a live birth.
- Women under 35 typically have higher pregnancy rates and fewer complications.
- With advanced maternal age (35+), there’s a greater risk of chromosomal abnormalities, which can lead to birth defects or miscarriage.
- Egg freezing is an option for women who want to delay pregnancy but preserve egg quality.
Early evaluation can help you decide the best time to start or continue fertility treatments.
2. Maintain a Healthy BMI
A stable and healthy BMI supports hormone balance, ovulation, and embryo implantation.
- A high BMI may reduce how your body responds to fertility medications and lower the success of an IVF cycle.
- A low BMI can affect egg production and hormone progesterone levels, making it harder for the fertilized egg to attach to the uterine lining.
- Obesity is linked to higher chances of miscarriage, poor embryo quality, and gestational diabetes.
Even small weight adjustments (5–10%) before treatment can make a big difference.
3. Use Preimplantation Genetic Testing (PGT)
PGT checks embryos for genetic problems before transfer. This helps avoid failed implantation or miscarriage caused by abnormal embryos.
- PGT-A (for aneuploidy) looks for missing or extra chromosomes, a common cause of IVF failure.
- It’s especially helpful for couples with recurrent pregnancy loss, advanced maternal age, or repeated IVF failures.
- Using PGT improves IVF success rates and allows for safe single embryo transfer, lowering the risk of multiple births.
Although it adds cost, it can increase the efficiency of a single IVF cycle.
4. Prioritize Single Embryo Transfer (SET)
Transferring one high-quality embryo reduces risks linked to twins or triplets.
- Multiple embryos may seem like a way to increase success, but they raise the chance of preterm birth and low birth weight.
- Singleton pregnancies are generally healthier for both mother and baby.
- SET is safer and now more effective thanks to embryo freezing and preimplantation genetic screening.
SET also avoids ethical and medical concerns linked to multifetal pregnancy reduction.
5. Choose a High-Quality IVF Clinic
Not all clinics offer the same level of care or success. Your choice can affect everything from lab quality to pregnancy rates.
- Look for clinics with high success in your age group and condition.
- Ask if they follow safety protocols like infectious disease screening and use the latest lab techniques (e.g., time-lapse monitoring).
- A strong clinic will also guide you through options like ICSI, donor eggs, or frozen embryo transfer based on your case.
Transparency about pricing, lab quality, and procedures is a good sign.
6. Ensure Proper Sperm Quality
Male fertility is just as important as female factors in IVF success.
- Poor sperm can lead to fertilization failure, poor embryo development, or even early miscarriage.
- Semen analysis checks for sperm abnormalities, such as low count or poor movement.
- If needed, ICSI (Intracytoplasmic Sperm Injection) is used to directly inject sperm into a mature egg, especially in cases of male factor infertility.
Lifestyle changes, supplements, or donor sperm are also valid paths when needed.
7. Avoid Smoking, Alcohol, and Toxins
Environmental and lifestyle factors strongly impact fertility and embryo quality.
- Smoking reduces egg and sperm quality and increases the risk of miscarriage and birth defects.
- Alcohol disrupts hormone balance and may affect embryo growth.
- Exposure to chemicals (e.g., pesticides, plastics) can interfere with reproduction.
Clearing these risks early improves the chances of a healthy live birth.
8. Optimize Timing of Embryo Transfer
The embryo must be transferred when the uterus is ready—this timing is critical.
- The hormone progesterone prepares the uterine lining for the fertilized egg to attach.
- If timing is off, even a healthy embryo won’t implant.
- Some clinics offer personalized timing using endometrial receptivity tests.
Proper timing gives embryos the best environment to grow into a successful pregnancy.
Want the Most Out of IVF?
Taking a smarter, more informed approach to your IVF journey increases your chance of success. These eight strategies don’t guarantee results, but they help reduce risk, improve IVF success rates, and give you a better shot at a healthy baby.
When IVF Fails: What’s Next? Options After an Unsuccessful Cycle
An unsuccessful IVF cycle can feel heartbreaking, but it doesn’t mean the end of the road. Many couples go on to have healthy pregnancies after adjusting their approach or exploring other options.
First, review what happened in the failed cycle with your doctor:
- Were there issues with egg quality, sperm health, or embryo development?
- Did the embryo fail to implant or was the uterine lining not ideal?
- Were hormone levels or timing slightly off?
Based on your results, here are common next steps:
- Try another IVF cycle with a modified protocol or different fertility medications
- Use preimplantation genetic testing (PGT) to select the healthiest embryos
- Consider using donor eggs, donor sperm, or frozen embryos if needed
In some cases, your doctor may suggest other paths:
- Explore other assisted reproductive technology like ICSI or frozen embryo transfer (FET)
- Look into surrogacy if carrying the pregnancy is a challenge
- Take a short break to focus on health, lifestyle, or emotional recovery
A failed IVF attempt is hard, but it often provides valuable insight. With the right changes and support, many couples succeed on their next try.
Real Patient Journeys: IVF at Dr. Anshu Agarwal’s Clinic

Every IVF journey is deeply personal — filled with emotions, doubts, and decisions. At Dr. Anshu Agarwal’s fertility clinic, we’ve had the privilege to support thousands of couples as they turned uncertainty into new beginnings.
Here are just a few real stories that show what’s possible with the right care, the right science, and the right team by your side.
Riya & Mohit: From Three Failed Cycles to a Baby Boy
Riya and Mohit had already been through three IVF attempts elsewhere — each one ending in disappointment. They came to Dr. Anshu Agarwal feeling emotionally drained and financially stretched.
- After a detailed review, Dr. Agarwal suggested using preimplantation genetic screening to improve embryo selection.
- A mild stimulation protocol was used to match Riya’s hormonal profile and preserve egg quality.
- On their very first cycle here, they had one healthy embryo transferred — and it worked.
Today, they’re proud parents of a baby boy. “We didn’t feel like just another case. Dr. Anshu took the time to understand us,” said Riya.
Neha: Beating the Odds at 40 with Her Own Eggs
Neha had been told her only option was an egg donor — due to her age and low ovarian reserve. But at Dr. Anshu Agarwal’s clinic, she got a second opinion and a chance to try one personalized cycle with her own eggs.
- Advanced lab support and close hormone progesterone tracking helped time her embryo transfer perfectly.
- A single embryo was transferred to reduce the risk of multiple births.
Nine months later, Neha delivered a healthy baby girl. “I almost gave up. Dr. Anshu gave me back hope—and science did the rest.”
Amit & Priya: Male Factor Infertility, Real Answers
After years of trying, tests showed male factor infertility was the primary issue. Sperm count was low, and natural conception wasn’t likely. They chose Dr. Anshu Agarwal based on her success with complex IVF cases.
- The clinic used ICSI (Intracytoplasmic Sperm Injection) to directly inject the best sperm into the egg.
- The couple was counseled on realistic expectations, supported through every step, and never rushed.
They now recommend the clinic to every couple they know. “Dr. Anshu’s team made us feel seen, heard, and supported like family.”
Why Choose Dr. Anshu Agarwal’s IVF Clinic?
Here’s what sets us apart:
- Personalized treatment based on your medical, emotional, and financial needs
- Advanced lab facilities with strict safety and infectious disease screening protocols
- Transparent pricing, honest advice, and consistently strong pregnancy rates
- Support for both common and complex infertility cases, including advanced maternal age, PCOS, and recurrent miscarriage
Whether you're planning your first IVF cycle or looking for hope after failed attempts, our clinic is ready to walk with you—every step of the way.
Your journey is unique. Your care should be too.
At Dr. Anshu Agarwal’s clinic, we combine world-class reproductive science with compassionate care that truly listens. Book a consultation today and take your first step toward the family you’ve been waiting for.
Your story could be next. Whether it’s your first cycle or your fifth, you don’t have to do it alone—reach out today.
How to Choose the Right IVF Clinic for Successful Treatment

Choosing the right IVF clinic isn’t just a box to check—it can directly impact your success, safety, and peace of mind. The wrong clinic can waste time, money, and energy. The right one can change everything.
1. Check Clinic Success Rates
Don’t just ask “what’s your success rate?” Ask for the full picture.
- Look at live birth rates, not just positive pregnancy tests.
- Ask for age-specific results. A 35-year-old and a 42-year-old don’t have the same odds.
- If using donor eggs or dealing with male factor infertility, ask about success in those cases.
Also ask how many single IVF cycles it usually takes to reach pregnancy.
2. Verify Accreditation and Certifications
A clinic with proper accreditation follows safety rules, clean lab practices, and government guidelines.
- Ask if they are certified by recognized fertility boards or national authorities.
- Accredited labs are required to meet quality control for things like embryo freezing, oocyte retrieval, and infectious disease screening.
It’s a basic but crucial safety step that protects your health and embryo quality.
3. Review the Experience of Doctors and Staff
IVF success depends heavily on the doctor’s experience—especially in complex cases.
- Ask how many years they’ve been practicing reproductive medicine.
- Have they worked with advanced maternal age patients, failed cycles, or rare conditions like endometriosis or PCOS?
- Do they personalize care or follow a strict one-size-fits-all routine?
Also observe how the staff communicates—are they clear, warm, and responsive?
4. Evaluate Lab Technology and Equipment
Most of IVF happens behind the scenes—in the lab. So the quality of the lab directly affects success.
- Ask if they use modern tools like ICSI, time-lapse embryo monitoring, and advanced incubators.
- Good labs can monitor embryo development, prevent contamination, and improve pregnancy rates.
- Do they track embryo status daily? Do they offer assisted embryo hatch if needed?
A strong lab can turn average embryos into viable pregnancies.
5. Look for Personalized Treatment Plans
IVF isn’t one-size-fits-all. Your treatment should be based on your unique profile: age, hormone levels, egg reserve, and health.
- Ask how they tailor fertility medicines and stimulation protocols to reduce risks like OHSS or failed cycles.
- Do they suggest SET or transfer multiple embryos without proper evaluation? That’s a red flag.
If they hand you a generic plan after one appointment, look elsewhere.
6. Ask About Support Services (Counseling, Nutrition, etc.)
IVF is not just physical—it’s emotional and mental too. Support matters.
- Does the clinic offer fertility counseling, emotional support, or referrals to specialists?
- Do they provide advice on lifestyle factors, diet, sleep, or mental health during treatment?
- Is there a nutritionist or support staff trained in IVF patient care?
Clinics that treat the whole person—not just the uterus—get better outcomes.
7. Understand the Cost and Financing Options
A high price doesn’t mean high quality, and a low price might hide missing services.
- Ask for a full breakdown: consultations, scans, medications, lab work, embryo storage, freezing, ICSI, etc.
- Does the price include one full cycle or just parts of it?
- Are there payment plans, refunds, or shared-risk programs?
Don’t wait until you're deep in the process to discover surprise fees.
8. Read Patient Reviews and Testimonials
Reviews show how the clinic treats people—not just embryos.
- Look beyond ratings. Read real patient stories, especially those who had similar challenges to yours.
- Are people mentioning clear communication, empathy, and thorough follow-ups?
- Do any mention staff being dismissive or pushy?
Word-of-mouth is often the most honest feedback.
9. Assess Clinic’s Experience with Specific Cases
Not all clinics specialize in all conditions. Pick one that’s skilled in your situation.
- Are they experienced with older patients, egg donors, male factor infertility, or PGT cases?
- Do they understand rare issues like thin uterine lining, immune factors, or repeated implantation failure?
A good match means higher chances of success and fewer trial-and-error cycles.
10. Check Availability of Advanced Options Like PGT and Embryo Freezing
Tech tools like preimplantation genetic testing (PGT) and embryo freezing improve safety and timing.
- Can they freeze embryos without damaging them? Ask about their success with thawed embryo transfers.
- Do they offer PGT for screening chromosomal issues?
- Can they track embryo development over time and choose the best for transfer?
These tools can help you achieve pregnancy faster—and more safely.
Final Word
Choosing the right IVF clinic can make or break your journey. Don’t rush. Ask questions. Compare options. And trust your gut. A great clinic won’t just promise success—they’ll prepare you for it.
Looking for IVF treatment in Ranchi or Delhi? Dr. Anshu Agarwal’s IVF clinic combines medical excellence with true patient care.
Conclusion
You’ve taken the time to learn—now take the step that matters most.
Understanding IVF is the first move, but confidence comes from action. Whether you're just starting to explore your options or are already considering next steps, don’t stay stuck in research mode.
You don’t have to figure it all out alone. Start asking questions, have real conversations, and lean into support. The path forward isn’t always clear—but it begins with showing up for yourself, fully informed and ready.
You’ve read, learned, and reflected—now take one empowered step forward. Talk to our team, and let’s explore your next move together.

.jpg)
.jpg)

.jpg)


