Worried that hypothyroidism in pregnancy might stop you from having a healthy baby? You're not alone, and the truth is—many women with an underactive thyroid go on to have a completely successful pregnancy with hypothyroidism, with the right care.
Roughly 2 to 3% of pregnant women experience hypothyroidism, most often due to Hashimoto's disease, according to the American Thyroid Association. What really matters is catching it early, managing your thyroid hormone levels, and getting regular checkups.
In this guide, we’ll walk through everything—from spotting symptoms to choosing the right thyroid hormone medication. You’ll also understand how your condition might affect your baby’s thyroid, and what steps help protect both of you.
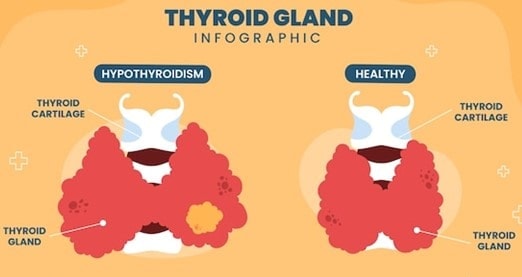
What Is Hyperthyroidism in Pregnancy?

Hyperthyroidism in pregnancy happens when your thyroid gland makes too much thyroid hormone. This speeds up your body’s metabolism more than it should, which may affect how you feel and how your pregnancy progresses.
It’s usually caused by an autoimmune disorder called Graves disease. Your immune system mistakenly attacks the thyroid, causing thyroid hormone production to go into overdrive.
According to the American Thyroid Association, 0.1% to 0.4% of pregnant women are affected by this condition. That may sound small, but thyroid dysfunction at any level needs attention—especially early in pregnancy.
How Does Maternal Hypothyroidism Affect You and the Baby?
Maternal hypothyroidism may seem silent at first, but it can affect your pregnancy if untreated. The risk of adverse pregnancy outcomes, like gestational hypertension or delayed fetal growth, becomes higher. That’s why checking thyroid function tests early in pregnancy really matters.
How Does Hyperthyroidism Affect Pregnancy Outcomes?
- Hyperthyroidism means your body is making too much thyroid hormone, which can strain your heart, metabolism, and baby’s development. The cause is often autoimmune thyroid disease, like Graves disease, where your immune system overstimulates the thyroid cells.
- If left untreated, untreated hyperthyroidism may lead to high blood pressure, miscarriage, or thyroid storm—a rare but serious complication during delivery. According to the American Thyroid Association, early screening can reduce risks of preterm birth and fetal growth restriction.
- Doctors will track your serum TSH, thyroid hormone requirements, and adjust treatment to help maintain normal thyroid function.
Possible complications include:
- Maternal side effects: rapid heartbeat, muscle cramps, anxiety
- Fetal risks: low birth weight, fetal thyroid dysfunction, increased risk of stillbirth
- Pregnancy complications: gestational hypertension, adverse pregnancy outcomes, and irregular menstrual periods postpartum
Medications like antithyroid drugs or radioactive iodine (not during pregnancy) are used carefully. You’ll likely need regular blood tests to stay on track. Every situation is different—talk to your doctor and trust that treatment works when closely monitored.
How Does Hypothyroidism Impact the Baby’s Thyroid?

In early pregnancy, your baby relies entirely on your maternal thyroid hormone for growth. Their fetal thyroid doesn’t start functioning until week 12 and doesn’t produce enough thyroid hormone until around week 18–20.
That’s why even subclinical hypothyroidism or too little thyroid hormone from the mother can impact brain development. According to WHO, early treatment prevents long-term cognitive impairments in children born to mothers with pregnancy hypothyroidism.
A delay in treatment or untreated hypothyroidism may cause the baby’s thyroid to underperform. This increases chances of low IQ, delayed milestones, or autoimmune thyroiditis later in life.
How maternal hypothyroidism affects the baby:
- Disrupts thyroid hormone production in the fetus
- Can impair maternal and fetal health if thyroid hormone replacement therapy is not started
- May result in stored thyroid hormone being inadequate for development
Doctors recommend adjusting thyroid hormone replacement dosage throughout pregnancy. Monitoring thyroid hormone requirements with regular thyroid testing is key.
Your doctor may also check for thyroid antibodies or tsh receptor antibodies to evaluate deeper causes. Being proactive helps prevent severe hypothyroidism in both you and your baby.
"Have questions about managing thyroid health during pregnancy? Schedule a consultation with Dr. Anshu Agarwal and get expert care tailored to your unique needs."
What Causes Hypothyroidism During Pregnancy?
Not all cases of hypothyroidism during pregnancy start during pregnancy itself. Sometimes it’s already there but hasn’t been diagnosed. Other times, changes in your body uncover an issue you didn’t know existed.
Let’s look at the most common causes:
1. Hashimoto’s Thyroiditis
This is the most common cause. It’s an autoimmune thyroid disorder where your immune system slowly destroys thyroid tissue.
- Often develops quietly before pregnancy
- Leads to long-term thyroid hormone deficiency
- Can result in subclinical hypothyroidism without obvious symptoms
2. Iodine Deficiency
Your body needs iodine to produce thyroid hormones. If you’re not getting enough, your thyroid can’t keep up—especially during pregnancy when demands increase.
- WHO recommends 250 mcg/day of iodine during pregnancy
- Too little may lead to mild hypothyroidism or even go unnoticed
- Severe deficiency affects both you and your baby’s thyroid
3. Thyroid Surgery or Radiation History
If you’ve had part or all of your thyroid removed, or had radioactive treatments, your thyroid might not work at full capacity anymore.
- You’ll need thyroid hormone replacement therapy before and during pregnancy
- Missed follow-up can lead to pregnancy hypothyroidism
- Common in thyroid cancer patients
4. Medications That Affect Thyroid Function
Certain medications can interfere with thyroid hormone levels, especially during early pregnancy.
- Lithium (used for mental health) may suppress thyroid
- Amiodarone and interferon also impact thyroid hormone production
- Always review your prescriptions with your doctor
5. Existing Hypothyroidism Before Pregnancy
If you were already on thyroid medicine, pregnancy can change your body’s needs.
- You may need higher doses to meet thyroid hormone requirements
- Unadjusted levels may lead to pregnancy symptoms like fatigue or weight gain
- Doctors monitor TSH and free T4 closely in early weeks
6. Pituitary Gland Disorders
Though rare, issues with the pituitary can affect thyroid stimulating hormone (TSH) levels.
- Low TSH leads to underactive thyroid even if the thyroid gland is fine
- Often linked with called thyroid stimulating immunoglobulin abnormalities
- May require endocrinologist-led care
Understanding these causes helps you manage things early. As the American Thyroid Association notes, “Early detection and treatment are key to reducing complications in mother and baby.”
"Early testing can make a real difference. Visit Dr. Agarwal’s clinic to get your thyroid function assessed before or during pregnancy."
What Are the Symptoms of Hypothyroidism in Pregnancy?

Hypothyroidism during pregnancy can be hard to spot at first. That’s because many symptoms overlap with regular pregnancy symptoms—like tiredness, mood shifts, or weight gain. But knowing what’s normal and what’s not can help you take action early.
The signs may be subtle, but they’re important. According to the American Thyroid Association, even mild hyperthyroidism or hypothyroidism can lead to issues if left undiagnosed. So if something feels off, it’s worth checking in.
- Fatigue and Weakness - You may feel exhausted even after resting. Muscles may feel sore or heavy, especially in the legs.
- Constipation - Sluggish digestion is common with low thyroid hormones play a role in regulating gut movement. It may worsen if iron supplements are involved.
- Weight Gain or Difficulty Losing Weight - Some weight gain is normal, but unexplained increases could signal subclinical hypothyroidism. This often goes unnoticed unless tested.
- Cold Intolerance - If you're always reaching for an extra blanket while others aren’t, take note. Your human chorionic gonadotropin levels can affect metabolism, and low thyroid function may be part of that imbalance.
- Dry Skin and Hair - Flaky skin, brittle nails, or shedding hair are early warning signs. Thyroid function affects hydration and cell turnover.
- Depression or Mood Changes - Mood swings may not just be hormonal. Treating hypothyroidism early can reduce risks of postpartum depression, according to Mayo Clinic data.
- Slow Heart Rate - A heart rate that drops below 60 bpm may be linked to low thyroid output. Report any dizziness or chest heaviness.
- Memory Issues or Trouble Concentrating - Often called “pregnancy brain,” this can also signal deeper thyroid-related fog. Watch for persistent forgetfulness.
- Puffy Face or Swelling - Facial puffiness—especially around the eyes—is one of the less talked about signs. It’s often mistaken for water retention.
- Hoarseness - A raspy or weak voice might not just be fatigue. Inflammation in the thyroid gland can press on the vocal cords.
Even if you’re unsure, regular screening matters. One quiet issue like overt and subclinical hypothyroidism can create real consequences—for both you and your baby. Always check with your doctor if symptoms persist.
Can You Have a Healthy Pregnancy with Hypothyroidism?
Yes, you absolutely can—but it depends on catching it early and staying consistent with treatment. Many women with even subclinical hyperthyroidism or hypothyroidism go on to deliver healthy babies without complications.
A study published in The Journal of Clinical Endocrinology & Metabolism found that with proper thyroid care, pregnancy outcomes were similar to those in women without thyroid disorders.
What helps the most:
- Taking levothyroxine as prescribed
- Getting your thyroid levels checked regularly
- Talking to your doctor if symptoms change
With support and monitoring, a healthy pregnancy is within reach.
"Dr. Agarwal specializes in caring for women with thyroid-related pregnancy concerns. Learn more about her high-risk pregnancy care and how she supports both mother and baby."
What Does the American Thyroid Association Recommend for Expecting Moms?
The American Thyroid Association (ATA) recommends that TSH levels stay below 2.5 mIU/L in the first trimester, and under 3.0 mIU/L in the second and third. This helps protect your baby’s brain development and lowers risk of pregnancy complications.
Women already on thyroid medication should increase their dose by about 30% as soon as pregnancy is confirmed, according to ATA guidelines.
Other key recommendations:
- Start treatment immediately after diagnosis
- Repeat thyroid function tests every 4–6 weeks
- Never skip follow-up visits during pregnancy
Following these steps can help ensure both maternal and fetal health.
How Is Hypothyroidism Diagnosed During Pregnancy?
If you’re pregnant and feeling more tired than usual, it might not just be pregnancy fatigue. Thyroid dysfunction—even if mild—can affect how you feel and how your baby develops. That’s why early testing matters.
Most doctors screen based on symptoms or risk factors. But if you have a history of thyroid surgery, autoimmune thyroiditis, or irregular menstrual periods, your doctor may test you right away.
The Main Test: Thyroid Function Tests
These blood tests help your provider check if your thyroid is underactive. They're simple and usually done early in the first trimester.
Key markers include:
- TSH (Thyroid Stimulating Hormone): High levels may suggest your thyroid is sluggish.
- Free T4: Measures the amount of usable thyroid hormone in your blood.
- Thyroid antibodies: If positive, could indicate autoimmune thyroid disease like Hashimoto’s.
The American Thyroid Association recommends keeping TSH levels below 2.5 mIU/L in the first trimester.
When Is Testing Needed?
Not everyone is tested routinely—but it should be considered if you:
- Have had radioactive iodine therapy
- Have subclinical hyperthyroidism or other known thyroid issues
- Are on thyroid hormone replacement therapy
- Had past pregnancy symptoms like early miscarriage or gestational hypertension
Why Timing Matters
Testing in the first trimester is important because your baby relies on your maternal thyroid hormone supply early on. Missing it can lead to fetal thyroid underdevelopment or adverse pregnancy outcomes.
“Routine thyroid screening may not be done in all pregnancies, but high-risk individuals should always be tested.”
— American College of Obstetricians and Gynecologists (ACOG)
If anything seems off, your doctor may repeat blood tests every few weeks. Don’t wait for symptoms to show up—hypothyroidism often starts quietly.
"Want trusted answers on thyroid and pregnancy care? Go to www.dranshuagarwal.com for expert advice, patient resources, and appointments."
Can an Overactive Thyroid or Graves Disease Complicate Pregnancy?

Yes, an overactive thyroid—especially caused by Graves disease—can create complications during pregnancy if not managed well. Graves is an autoimmune condition where the body produces antibodies that overstimulate the thyroid gland, leading to too much thyroid hormone.
This can speed up your heart rate, affect weight, and disrupt your baby’s growth if left unchecked. Most issues happen when the condition goes undiagnosed or treatment isn’t adjusted for pregnancy.
Possible Risks with Untreated Hyperthyroidism:
- Miscarriage or preterm birth
- Low birth weight or fetal thyroid overactivity
- Preeclampsia or gestational hypertension in the mother
- Rarely, thyroid storm during labor—a dangerous surge of hormone levels
Doctors usually monitor thyroid hormone levels and TSH frequently during each trimester. If needed, antithyroid medications like propylthiouracil may be prescribed in early pregnancy, with methimazole often used later.
After delivery, some women with Graves disease may experience postpartum thyroiditis. This temporary condition starts with a hyperthyroid phase followed by a hypothyroid phase. It can be tricky to distinguish from postpartum fatigue or depression, so follow-up care is important.
“Women with autoimmune thyroid disease should be monitored closely both during and after pregnancy.”
— American Thyroid Association
The good news? With early diagnosis, safe medication, and consistent monitoring, most women with Graves disease can have healthy pregnancies and recover well postpartum.
Dr. Anshu Agarwal About the Role of Iodine Deficiency in Thyroid Health During Pregnancy?

Dr. Anshu Agarwal is a distinguished gynecologist and obstetrician based in Ranchi, India, with over 18 years of experience in women's health. She specializes in high-risk obstetrics, infertility treatments, and laparoscopic surgeries.
Dr. Agarwal has served as a Senior Resident at Safdarjung Hospital, New Delhi, and currently practices at Paras HEC Hospital in Ranchi. Her commitment to patient care and extensive expertise make her a trusted name in maternal health.
Iodine is a vital nutrient for thyroid hormone production, especially during pregnancy. Dr. Agarwal emphasizes the importance of adequate iodine intake for expecting mothers to ensure optimal thyroid function and fetal development.
Key Insights:
- Increased Iodine Requirements: Pregnant women need about 250 micrograms of iodine daily to support increased thyroid hormone production.
- Risks of Deficiency: Iodine deficiency during pregnancy can lead to complications such as miscarriage, stillbirth, and developmental delays in children.
- Dietary Sources: Incorporating iodine-rich foods like dairy products, seafood, eggs, and iodized salt can help meet daily requirements.
- Supplementation: Dr. Agarwal advises that prenatal vitamins should contain at least 150 micrograms of iodine to prevent deficiency.
- Monitoring Thyroid Function: Regular thyroid function tests are crucial during pregnancy to detect and manage any thyroid dysfunction early.
By ensuring adequate iodine intake and monitoring thyroid health, expecting mothers can promote a healthy pregnancy and support their baby's development.
Can Thyroid Problems Show Up After Delivery?
Yes, thyroid issues can develop even after childbirth—this is known as postpartum thyroiditis. It often starts with a short period of overactive thyroid symptoms like anxiety and palpitations, followed by an underactive thyroid phase with fatigue and low mood.
Many women mistake it for regular postpartum changes. But according to the American Thyroid Association, about 1 in 20 women experience it within the first year after delivery.
What to watch for:
- Unexplained weight changes
- Mood swings or brain fog
- Heart rate changes
Early testing helps prevent long-term complications.
FAQs on Hyperthyroidism During Pregnancy
1. Can thyroid affect pregnancy test results?
- Not directly. Hyperthyroidism doesn’t interfere with the hormones that pregnancy tests detect, such as hCG. However, if thyroid symptoms like missed periods or fatigue overlap with early pregnancy signs, it may cause confusion.
- If you're unsure, confirm with a blood test and talk to your doctor about your thyroid levels alongside your pregnancy status.
2. Can thyroid transfer from mother to baby?
- Not the thyroid itself, but certain thyroid antibodies, especially in Graves disease, can cross the placenta. These may temporarily affect the baby’s thyroid function.
- That’s why doctors monitor fetal growth and may perform fetal thyroid ultrasounds if needed.
3. What is a normal thyroid level in pregnancy?
- The American Thyroid Association recommends keeping TSH (thyroid stimulating hormone) below 2.5 mIU/L in the first trimester, and under 3.0 mIU/L in the second and third.
- Your doctor may adjust your medication to stay within this range. Consistent monitoring every 4–6 weeks is key to protecting both mother and baby.
4. What are bad habits for the thyroid?
Some daily habits can stress your thyroid more than you realize. These include:
- Skipping thyroid medication or taking it inconsistently
- Overconsumption of raw cruciferous vegetables (like cabbage or broccoli)
- Not getting enough iodine through diet or supplements
- Chronic stress, which disrupts the immune system and may worsen autoimmune thyroid conditions
- Self-adjusting medication without medical advice
Small lifestyle tweaks can support better thyroid health long-term.
5. How to get pregnant with thyroid problems?
Start by getting your thyroid hormone levels stable. Whether you have subclinical hyperthyroidism or another thyroid condition, untreated hormone imbalances can delay ovulation or increase miscarriage risk.
Steps to prepare:
- Work with an endocrinologist or OB-GYN familiar with thyroid care
- Take thyroid hormone replacement therapy exactly as prescribed
- Check for thyroid antibodies if you’ve had previous fertility issues
- Maintain regular thyroid function tests while trying to conceive
Once your levels are under control, many women with thyroid disorders go on to have healthy pregnancies. Always ask questions and stay involved in your care.
Conclusion
If you've been diagnosed with hypothyroidism, don’t panic—a successful pregnancy with hypothyroidism is absolutely possible. The key is to stay informed, stay consistent with treatment, and keep an open line of communication with your doctor. Managing your thyroid hormone levels early and throughout pregnancy helps protect both you and your baby.
You don’t have to navigate this alone. From recognizing symptoms to understanding lab results and making small lifestyle changes, each step plays a part. And if you ever feel unsure—ask. The more you understand your thyroid, the more confident you'll feel about your pregnancy journey.
Remember, many women with hypothyroidism during pregnancy go on to have healthy, full-term babies. With regular checkups, the right support, and a little patience, you can too.
You've got this—and we're right here with you every step of the way.


.jpg)

.jpg)


