Could something as silent as a weakening cervix quietly risk your entire pregnancy?
Most women have never even heard of an incompetent cervix—until it’s too late. It doesn’t cause pain. It doesn’t give warning. And for some, it leads to pregnancy loss without any signs.
This condition, also called cervical insufficiency, means your cervix opens too soon—often without symptoms. The result? Premature delivery, complications, or heartbreaking loss. But with early diagnosis and the right care, there’s hope.
In this article, you’ll get clear, expert-backed answers about incompetent cervix—what it is, how it’s diagnosed, and how treatments like cervical cerclage can help you carry your pregnancy safely.
What is an Incompetent Cervix (Cervical Insufficiency or Cervical Incompetence)?
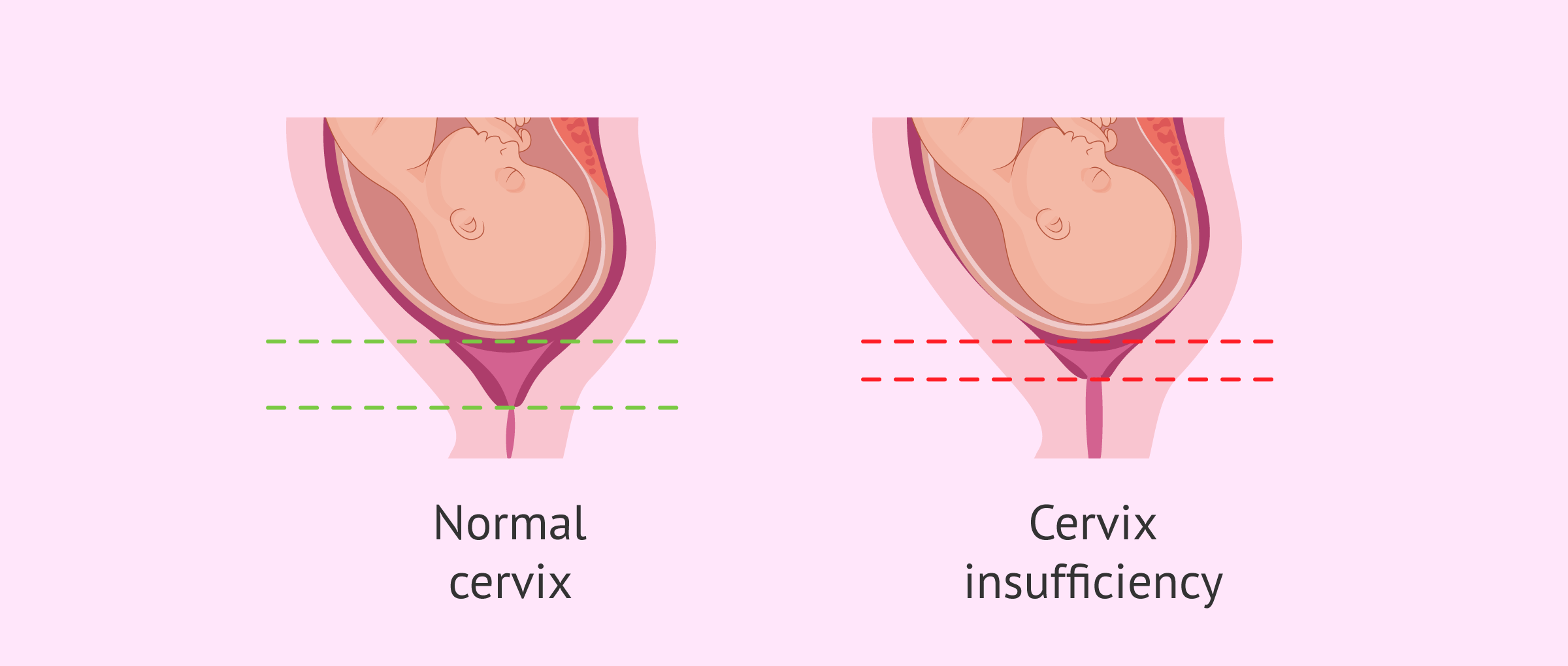
An incompetent cervix, also called cervical insufficiency, happens when the cervix opens too early during pregnancy without pain or contractions. This can lead to miscarriage or early birth, usually in the second trimester, before the baby is ready to survive outside the womb.
Understanding Cervical Weakness: Anatomy and Function of the Cervix
The cervix is the lower, narrow part of the uterus that connects to the vagina. It stays closed during pregnancy to hold the baby inside the womb.
As the pregnancy continues, the cervix slowly softens and opens near the end — this is normal and part of labor. But in some women, the cervix opens too early. This is called cervical weakness.
Cervical weakness means the cervix can’t stay strong enough to hold the baby for the full term. It may open without pain or contractions.
What the cervix normally does in pregnancy:
- Stays firm and tightly closed
- Supports the growing baby
- Slowly opens near labor time
What happens in cervical weakness:
- Cervix becomes soft too early
- Opens without any pain or signs
- Can lead to early delivery or pregnancy loss
Knowing how the cervix works helps doctors find problems early. If they see signs of cervical weakness, they can take steps to support the pregnancy.
10 Risk Factors for Incompetent Cervix and Cervical Insufficiency
Certain health issues, past surgeries, or body conditions can weaken the cervix. Knowing the risk factors early helps doctors plan steps to prevent pregnancy loss or preterm birth.
1. Previous Second-Trimester Pregnancy Loss
Women who’ve had a second trimester pregnancy loss may be at risk for an incompetent cervix. This often happens without warning and may repeat in future pregnancies.
- Losses during weeks 13–24 are often linked to painless cervical dilation.
- These cases are sometimes diagnosed after a pattern of trimester miscarriage.
- A short or weakened cervix may go unnoticed until it’s too late.
Doctors use your medical history to decide if you need closer monitoring or a prophylactic cerclage early in pregnancy.
2. History of Cervical Surgery (e.g., LEEP, Cone Biopsy)
Surgeries like LEEP, cone biopsy, or cervical conization can damage the cervical tissue or shorten the cervical canal.
- These can lead to cervical stenosis or weaken the support structure of the uterine cervix.
- If the cervix shortens or opens early in later pregnancies, it may be due to past treatments.
Women with this history often need transvaginal ultrasound scans to track cervical length in each pregnancy.
3. Uterine or Cervical Abnormalities
Birth defects or abnormal cervical structure can raise the chance of cervical incompetence.
- A patulous cervix or malformed uterus makes the cervix more likely to open early.
- These changes may not be noticed until a trimester delivery occurs unexpectedly.
Doctors might suggest cerclage procedures or close scanning, especially in high risk cases.
4. Trauma to the Cervix During Delivery or Procedures
Any injury or deep cut to the cervix can weaken it. This is known as cervical trauma.
- It may happen during difficult deliveries or D&C procedures.
- Scarred or damaged areas might not stay closed during the next pregnancy.
These women may need a therapeutic cerclage in early pregnancy to hold the cervix closed.
5. Multiple Pregnancies (Twins or More)
Carrying more than one baby adds extra pressure on the cervix.
- This weight can make the cervix begin to open earlier than it should.
- It increases the risk of spontaneous preterm birth and advanced cervical dilation.
Women expecting twins may get early ultrasounds to check for short cervix or early signs of preterm labour.
6. Connective Tissue Disorders (e.g., Ehlers-Danlos Syndrome)
Conditions that affect the body’s support tissues can also weaken the cervix.
- Ehlers-Danlos makes tissue too stretchy, including the cervical canal.
- This can lead to early cervical dilation, even in the first trimester.
Doctors may suggest a prophylactic cervical cerclage to prevent early opening in these cases.
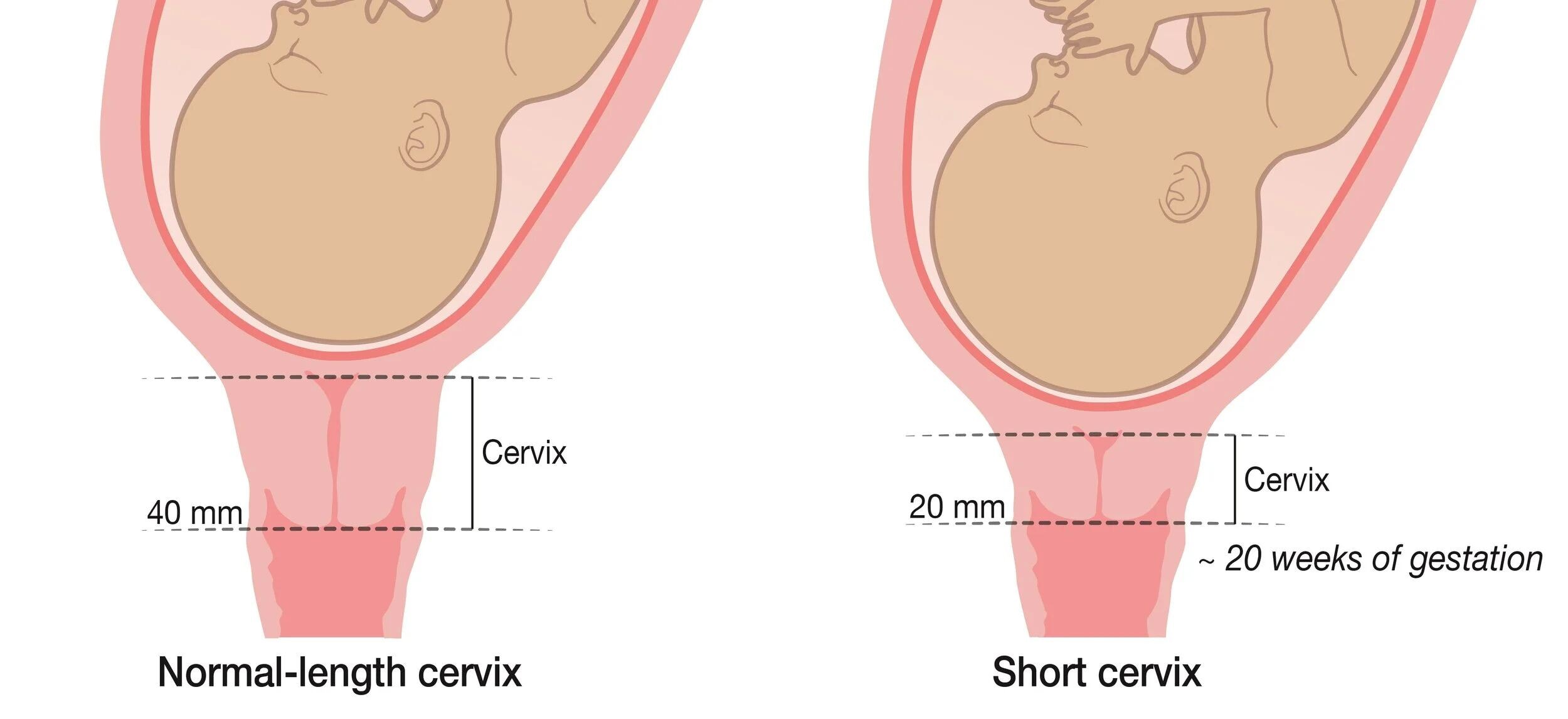
7. Short Cervix Detected in Early Ultrasound
A short cervix (measured in mm) is one of the top warning signs of cervical insufficiency.
- It’s often found during transvaginal ultrasonography in the second trimester.
- A cervical length below 25 mm increases the risk of premature birth or preterm delivery.
Treatment may include vaginal progesterone or bed rest depending on how early the shortening starts.
8. Family History of Cervical Insufficiency
If your mother or sister had issues with the cervix opening early, your chances may be higher.
- This may be linked to inherited tissue weakness or body structure.
- Your doctor will watch for other signs, especially in past pregnancies.
Early planning helps prevent pregnancy loss from recurring due to weak cervix.
9. Prior Use of Cervical Cerclage in Pregnancy
If you’ve had a cervical stitch or cerclage procedure before, it’s a clue that your cervix may need extra support again.
- Your doctor may plan a prophylactic cerclage early in the new pregnancy.
- Regular checks help spot signs like pelvic pressure, ruptured membranes, or early uterine contractions.
This lowers your risk of preterm birth in subsequent pregnancies.
10. Exposure to Diethylstilbestrol (DES) in Utero
Women whose mothers took DES (a drug used in the past) during pregnancy may have cervix problems.
- It can cause a weak or underdeveloped cervix.
- These women are more prone to second trimester miscarriages and incompetent cervix cause problems.
Regular lab tests and ultrasound checks are often part of care for women with this exposure history.
How an Incompetent Cervix Cause Problems During Pregnancy
An incompetent cervix can quietly open too early during pregnancy, causing serious problems. These issues often happen in the second trimester, before the baby is ready to survive outside the womb.
Let’s look at the most common ways it can affect both mother and baby.
1. Increased Risk of Pregnancy Loss in the Second Trimester
When the cervix opens early, the pregnancy may end before the baby can survive. This is a leading cause of second trimester miscarriage.
- Many cases happen without pain or warning.
- This is often seen in women with a previous pregnancy loss.
- Early care and support may help prevent premature birth in the future.
Doctors in maternal fetal medicine often guide women with this history through special care plans.
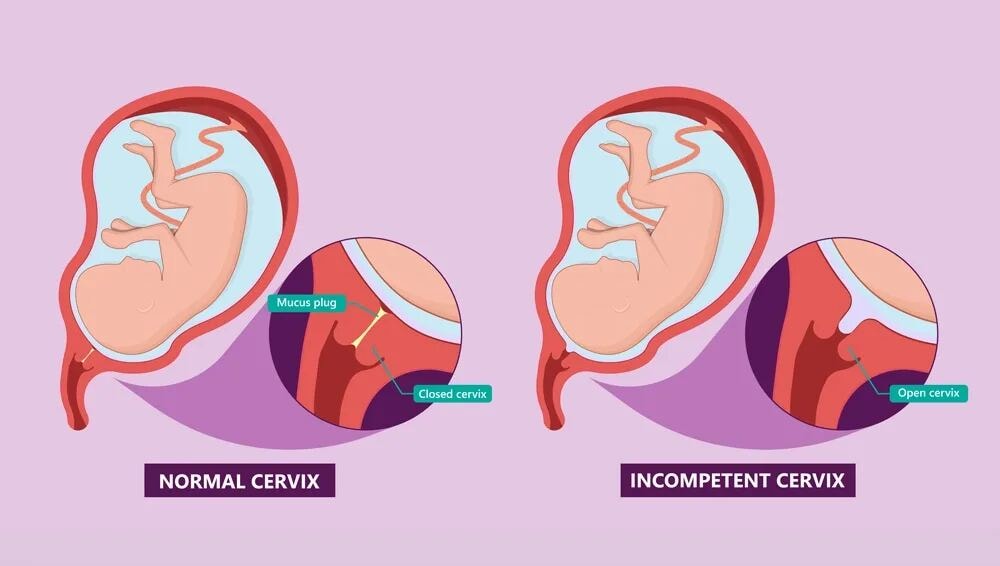
2. Painless Cervical Dilation Without Contractions
One sign of cervical incompetence is painless cervical dilation. The cervix opens without uterine contractions, making it harder to detect early.
- No bleeding, no pain — it just opens silently.
- This may lead to a fast pregnancy loss or need for a procedure called cerclage.
Monitoring cervical length through ultrasound helps spot this early.
3. Premature Rupture of Membranes (PROM)
When the amniotic fluid leaks before labor begins, it's called premature rupture.
- This can happen if the cervix opens and weakens the sac around the baby.
- PROM increases the chance of infection or uterine rupture in rare cases.
Early signs like vaginal discharge or wetness should be checked right away.
4. Preterm Labor and Delivery Before 37 Weeks
An open or short cervix makes preterm labor more likely. Labor can start before the baby is ready.
- This often leads to preterm birth, which may need NICU care.
- Babies born too soon may have breathing, feeding, or growth problems.
To reduce this risk, doctors may start progesterone treatment or suggest bed rest in high-risk cases.
5. Infection and Inflammation (Chorioamnionitis)
When the protective barriers break down early, bacteria can enter. This leads to chorioamnionitis, an infection of the sac around the baby.
- Signs include fever, vaginal bleeding, and pain.
- It can harm both baby and mother if not treated quickly.
Experts in reproductive medicine watch closely for these risks, especially after transabdominal cerclage or other cervical procedures.
6. Umbilical Cord Prolapse or Compression
When the cervix dilates early, the cord can slip down. This is called cord prolapse and it cuts off the baby’s oxygen.
- It is rare but very dangerous.
- Happens more often in early trimester delivery or multiple pregnancies.
Doctors act fast when this happens, usually by emergency delivery.
7. Fetal Growth Restriction Due to Early Delivery
If the baby is born too soon, they may be underweight or underdeveloped. This is known as fetal growth restriction.
- Can lead to breathing trouble or longer hospital stays.
- Prenatal vitamins and nutrition help, but timing of delivery matters most.
Staying healthy, keeping a healthy weight, and following medical advice can support a healthy pregnancy.
8. Emotional and Psychological Impact of Pregnancy Loss
The emotional toll of a pregnancy loss or early birth is often deep and lasting.
- Many women feel guilt, fear, or sadness in future pregnancies.
- Support from family, doctors, and groups like Fetal Medicine Foundation can help.
Knowing what to expect and how to prepare can ease some of this stress.
When to Seek Care: Symptoms and Early Warning Signs of Cervical Insufficiency

Cervical insufficiency often shows no signs until it's too late — but sometimes, your body gives small clues. Spotting these early can help prevent serious problems like preterm birth or pregnancy loss.
Here are some signs that should never be ignored during the second trimester:
- Sudden pelvic pressure, as if the baby is pushing down
- Vaginal discharge that’s watery, pink, or mixed with mucus
- Mild vaginal bleeding without pain or cramps
- A feeling of "heaviness" in the lower belly
- Backache or cramps that feel different from normal
- Increased urge to urinate or unusual discomfort down there
These symptoms don’t always mean there’s a problem, but they’re worth checking out — especially if you have other risk factors, like a previous second-trimester loss or known cervical weakness.
If you notice any of these, contact your doctor or maternal fetal medicine specialist right away. Early action can save your pregnancy.
How Is an Incompetent Cervix Diagnosed?

Diagnosing an incompetent cervix can be tricky because symptoms are often mild or missing. Doctors use a mix of your health history and simple tests to check if your cervix is at risk of opening too soon.
Here are the main steps used to find out if a cervix is weak or not doing its job.
1. Review of Obstetric and Surgical History
Your doctor will first look at your previous pregnancy records and any surgeries you’ve had.
- Losses in the second trimester may be a sign of a weak cervix.
- Surgeries like cone biopsy or LEEP can also damage the cervix.
- This step helps spot patterns and plan a procedure called cervical cerclage if needed.
Looking at your medical history gives the doctor early clues before other tests begin. It's often the first sign that you may need closer watch in the next pregnancy.
2. Transvaginal Ultrasound to Assess Cervical Length
A transvaginal ultrasound is the most trusted test to measure cervical length. It’s quick, painless, and gives a clear image.
- The cervix is measured in millimeters to see if it's too short.
- A short cervix (less than 25mm) may mean a higher chance of preterm birth.
- Doctors also check for funneling, where the inner part of the cervix starts to open.
This scan is often done in the second trimester and may be repeated in high-risk pregnancies.
3. Identification of Cervical Funneling or Opening
Sometimes, the top of the cervix starts to open while the outer part stays closed — this is called funneling.
- It can be seen on ultrasound before symptoms appear.
- This helps catch early warning signs before vaginal bleeding or pregnancy loss begins.
- It’s one of the most important signs of cervical insufficiency.
Funneling along with a short cervix may lead your doctor to suggest progesterone treatment or placing a cervical stitch.
4. Physical or Pelvic Examination (in Select Cases)
In some situations, a pelvic exam helps check for cervical dilation or softening.
- This is usually done if there's pelvic pressure, vaginal discharge, or pain.
- A soft or open cervix mid-pregnancy is a serious sign.
- Doctors check if the cervix is still firm, long, and closed.
If any changes are found, they may act quickly with a cerclage to prevent premature birth.
5. Diagnosis of Cervical Insufficiency After Unexplained Mid-Trimester Pregnancy Loss
Many women only learn they have a weak cervix after losing a baby in the second trimester.
- This is called a "diagnosis by history" because it’s based on past pregnancies.
- If a pattern is found, reproductive medicine experts may suggest a prophylactic cerclage in future pregnancies.
In addition to medical treatment, focusing on a healthy diet, prenatal vitamins, and regular scans can help build up strength for the next pregnancy.
6. Screening in High-Risk Pregnancies
If you’ve had a loss, surgery, or signs of cervical incompetence, you’re considered high risk.
- You may need frequent ultrasounds to track cervical length and funneling.
- Early treatment such as vaginal progesterone or cerclage procedures may be recommended.
This care is usually managed by a maternal fetal medicine specialist who monitors your condition closely for a healthy pregnancy.
Had a second-trimester loss or been told your cervix is short?
You deserve answers. Dr. Anshu Agarwal specializes in early diagnosis and prevention — before problems begin.
Adjunct Treatments for Cervical Weakness: Progesterone, Pessaries, and More
When a cervix starts to soften or shorten too early, some treatments can help avoid pregnancy loss or preterm birth — even without surgery. These extra methods are called adjunct treatments, and they often work alongside or instead of a cervical stitch.
1. Vaginal Progesterone

Progesterone is a hormone that helps the uterus stay calm and the cervix closed. Giving it early, especially as vaginal progesterone, may lower the risk of early delivery.
- It’s often used when a short cervix is found in a routine scan.
- Simple to use and usually taken daily.
- It’s safe for most women and doesn’t affect the baby.
2. Cervical Pessary
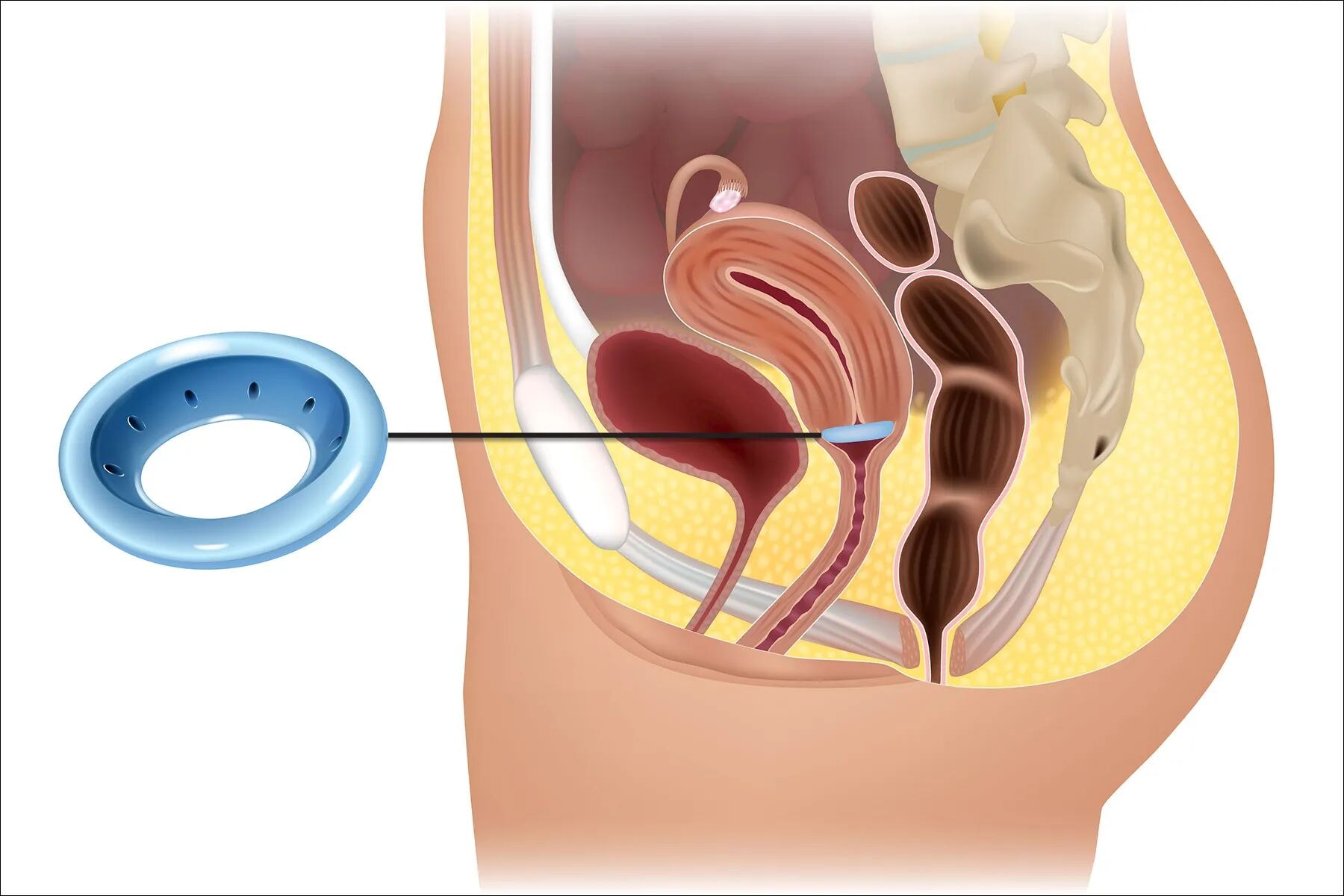
A pessary is a small, soft silicone ring placed inside the vagina to support the cervix from below. It's non-surgical and painless.
- Helps take pressure off the cervix in high-risk pregnancies.
- Sometimes used when women can’t get a prophylactic cerclage.
- Can be removed easily if symptoms change.
3. Activity Modification and Bed Rest

Some women may be advised to slow down or take bed rest, especially if the cervix is changing fast.
- Avoiding heavy lifting, long walks, or standing too long may reduce pressure.
- Not proven for everyone, but helpful in specific maternal fetal medicine cases.
- Always follow your doctor’s advice — rest may help, but it's not a cure.
4. Anti-inflammatory or Antibiotic Support

If there's any sign of infection or inflammation, doctors may treat it quickly.
- Infections can harm the amniotic fluid or weaken the cervical tissue.
- Medication helps protect both baby and mom in sensitive cases.
Tips Manage Pregnancy After Cervical Insufficiency Diagnosis
Being diagnosed with cervical insufficiency can be stressful — but the right care plan can protect both you and your baby. These tips are based on what doctors recommend to lower the risk of pregnancy loss or preterm birth.
1. Monitoring After Cervical Cerclage Placement
After a cervical stitch is placed, close monitoring is needed to make sure it's working.
- Your doctor may check for signs of infection, pressure, or discomfort.
- Regular visits help track any changes in your cervical length or stitch position.
- Some women may need bed rest if the cervix still shows signs of opening.
2. Attend All Scheduled Cervical Length Ultrasound Scans
Transvaginal ultrasound is the most accurate way to check your cervical length.
- If your cervix becomes shorter over time, it could lead to early labor.
- These scans help doctors act early — either by adjusting treatment or adding a second procedure called cerclage.
3. Limit Physical Activity as Advised (Including Bed Rest if Recommended)
Too much movement or pressure can cause the cervix to shorten faster.
- Doctors may recommend full or partial bed rest depending on your case.
- Avoid housework, climbing stairs, long walks, or standing for hours.
- Some may be asked to stop working or travel less.
4. Take Prescribed Medications Like Progesterone Consistently
Progesterone treatment, especially vaginal progesterone, is often used to help keep the cervix closed.
- It helps lower inflammation and reduce the risk of spontaneous preterm birth.
- Missing doses may reduce the benefit, so use it regularly and as directed.
5. Avoid Heavy Lifting, Intercourse, or High-Impact Activities
Activities that increase belly pressure or cause uterine tightening should be avoided.
- Lifting more than 5–10 kg can strain the weakened cervix.
- Sexual activity may be limited, especially after a cerclage procedure.
- Exercises like running or jumping can bring on uterine contractions.
6. Recognize and Report Warning Signs Early
Knowing what to look for helps you act quickly and avoid complications.
- Signs like vaginal bleeding, watery vaginal discharge, or cramps can mean early changes.
- You may also feel pelvic pressure or a dull backache.
- Any fluid leak could signal loss of amniotic fluid.
7. Prepare Emotionally and Practically for Possible Early Delivery
Even with treatment, some babies may come early. Planning ahead reduces panic and stress.
- Pack your hospital bag by 28–30 weeks and discuss preterm care options.
- Join a support group or talk to a counselor if you're feeling anxious.
8. Maintain Regular Communication with a High-Risk OB/GYN
Specialists in maternal fetal medicine have experience with cervical weakness cases.
- They monitor your pregnancy closely and adjust treatment as needed.
- You’ll likely have more check-ins than usual — sometimes weekly.
9. Consider Hospital Admission if Cervical Changes Progress
If the cervix shortens too fast or starts to open despite treatment, hospital care may be needed.
- In the hospital, doctors can monitor for signs of preterm labour or ruptured membranes.
- You may get steroids to help the baby’s lungs or IV meds to stop contractions.
10. Plan for Post-Cervical Stitch (Cerclage) Care and Follow-Up
Most cervical stitches are removed between 36–37 weeks — earlier if labor starts.
- After removal, you may deliver soon or carry full term.
- Doctors will watch for advanced cervical dilation or signs of labor.
Worried about your cervix during pregnancy?
Don’t wait for symptoms — book a proactive consultation with Dr. Anshu Agarwal and get a personalized care plan.
How Dr. Anshu Agarwal’s Approach Compares to Cleveland Clinic and Other Leading Institutions

When it comes to managing cervical insufficiency and preventing pregnancy loss, every detail matters — from early diagnosis to the timing of a cervical stitch. Both global leaders like Cleveland Clinic and trusted specialists like Dr. Anshu Agarwal follow evidence-based care.
But what sets Dr. Agarwal’s approach apart is her ability to combine medical precision with personalized care for Indian women.
Shared Standards with Leading Centers
Dr. Anshu Agarwal follows international guidelines similar to those used at Cleveland Clinic, including:
- Using transvaginal ultrasound to monitor cervical length
- Offering timely prophylactic cerclage in high-risk cases
- Prescribing vaginal progesterone for women with a short cervix
- Closely monitoring post-cerclage pregnancies through structured check-ups
These protocols are backed by top research and are proven to help prevent premature birth and support a healthy pregnancy.
What Makes Dr. Anshu Agarwal’s Care Unique
Where Dr. Agarwal adds even more value is through her focus on patient-first care:
- Local access to high-risk OB/GYN services without the need for big-city referrals
- More frequent cervical scans, especially for women with past trimester miscarriage
- Culturally sensitive advice on bed rest, activity limits, and family support
- A tailored approach to progesterone treatment, based on both medical and lifestyle factors
Her goal isn’t just to follow global best practices — it’s to adapt them to the individual needs of each woman, especially in Indian clinical settings where resources and support can vary.
Why This Matters for You
If you’ve been diagnosed with a weak cervix, or had a second trimester pregnancy loss, you need a care plan that’s not just medically sound but deeply personal. With Dr. Agarwal, you’ll get both: global-standard treatment and the kind of attention that only a hands-on specialist can offer.
In short — world-class care, closer to home.
Looking for expert care that blends science with compassion?
Dr. Anshu Agarwal offers world-class cervical insufficiency treatment — right here in Ranchi
Conclusion
Now that you’ve made it this far, take a moment to pause — not with fear, but with awareness. Pregnancy comes with unknowns, and it’s okay to feel unsure. What matters most is knowing that with the right steps, timing, and support, you're not powerless.
So ask questions. Keep learning. Trust your instincts. And if something feels off, speak up early. Your voice is one of the most powerful tools in protecting your pregnancy — use it.
Your pregnancy deserves expert care, not guesswork.
With 18+ years of experience, Dr. Anshu Agarwal provides trusted care for high-risk pregnancies — without the need to travel far.

.jpg)
.jpg)

.jpg)


