Is your biological clock ticking — or is it just the pressure talking?
If you’ve ever sat with that question, staring at a calendar or scrolling through fertility forums, you’re not alone. More and more women are turning to the AMH anti mullerian hormone test for answers. But is it really worth it? And how do you know if it’s meant for you?
This isn’t a one-size-fits-all test. It can be useful — or misleading — depending on your goals, age, and health history.
In this article, you'll learn exactly who should take the AMH anti mullerian hormone test, when to take it, and what the results actually mean — so you can move forward with clarity, not confusion.
What Is the AMH Test and Why It Matters for Fertility

The AMH test, or anti mullerian hormone test, is a simple blood test that measures the level of AMH in your body. This hormone is linked to how many eggs you have left — also known as your ovarian reserve.
Role of Anti Mullerian Hormone(AMH) in Reproduction

Anti Mullerian Hormone (AMH) is a natural signal made by small follicles inside the ovaries. This process is called AMH production and it starts early in life.
Doctors use it to assess ovarian function because it gives a picture of how many eggs are still inside the ovaries, a sign of your egg reserve or fertility potential.
- AMH is also known as mullerian inhibiting substance or müllerian inhibiting substance
- It is measured in ng ml, which is the unit shown on most lab reports
- AMH helps guide doctors before treatments like vitro fertilization
In a normal menstrual cycle, many small follicles grow, but only one egg usually matures. AMH comes from these small growing follicles, which is why AMH hormone levels give a better view of egg quantity than older tests like follicle stimulating hormone.
- Doctors often compare AMH with antral follicle count on ultrasound to get a fuller picture
- When AMH levels naturally decline with age, it points to a low ovarian reserve
- Knowing your AMH is especially useful if you’re planning pregnancy or egg freezing through vitro fertilization
AMH is not about quality of eggs but quantity. It reflects how your female reproductive organs (mainly the ovaries) are working at that time. By understanding AMH, doctors and patients can plan better for fertility and treatment options.
Want expert clarity on this topic? Connect with DrAnshuAgarwal today
7 Common Reasons Doctors Recommend the AMH Test

The AMH hormone test is more than just a number — it gives doctors helpful insight into how the ovaries are working. Below are seven common reasons they suggest this test to understand a woman’s overall reproductive health and fertility chances.
1. Assessing Ovarian Reserve
Knowing how many eggs are left in the ovaries is one of the main reasons this test is done. Doctors use it to estimate your egg count, which can guide fertility planning.
AMH is made by granulosa cell layers of small ovarian follicles. When AMH levels are low, it can suggest low ovarian reserve or ovarian aging, especially in women of advanced reproductive age.
- The test measures how much hormone is in your blood sample, shown in ng ml
- This gives clues about your remaining egg count, even before other symptoms show
- Along with the AMH test, doctors may do an antral follicle count to confirm the results
Understanding AMH early helps prevent surprises later, such as early menopause or missed chances for family planning.
2. Guiding Fertility Treatment Plans
The AMH hormone test is often part of the first step in planning infertility treatment or IVF treatment. It helps shape the strategy that works best for each person.
Women with higher AMH levels may respond better to injectable fertility drugs, while lower levels may need adjusted doses to protect the reproductive organs.
- It helps doctors prepare for how your body might react to treatments
- AMH gives a rough idea of how many eggs may grow during ovarian stimulation
- It's useful before someone starts undergoing treatment for fertility
This approach avoids trial and error and makes each step of the journey more focused and effective.
3. Evaluating Polycystic Ovary Syndrome (PCOS)
Women with PCOS often have a high egg number and more small follicles — this leads to higher AMH levels. So, the test can help point to PCOS when used alongside other signs.
In PCOS, measuring AMH levels supports diagnosis, especially when other hormone tests show mixed results.
- PCOS may also include signs of male hormones imbalance or male pattern baldness
- AMH helps avoid misdiagnosis by checking what's happening inside the ovaries
- It’s not a stand-alone diagnostic test, but it adds one more strong clue
This makes the AMH test useful in identifying PCOS early and managing it properly.
4. Predicting Response to Ovarian Stimulation
Before starting any IVF treatment, doctors need to know how the ovaries will react to medication. The AMH test helps predict this by showing how active the ovarian follicles are.
- It gives a safe estimate of ovarian response to injectable fertility drugs
- Higher AMH levels usually mean a stronger response, while lower levels may need extra care
- Helps avoid side effects like ovarian mass formation or overstimulation
This helps create a safer and more effective fertility plan.
5. Considering Egg Freezing or Fertility Preservation
Women thinking of freezing their eggs — whether due to personal goals, health issues, or age — benefit from this test. AMH shows how much time might be left before egg count or quality drops.
- It helps spot signs of premature ovarian failure or low reserve early on
- Doctors can suggest the best time for egg freezing before eggs decreases too much
- Useful for women who want kids later but aren't ready now
This test helps take action before fertility becomes harder to manage.
6. Monitoring Ovarian Function After Medical Treatment
Women who've had surgery, cancer care, or treatments that affect the ovaries can use the AMH test to check how much function remains. It tells if the reproductive organs are still active.
- AMH is used to track recovery or damage after chemotherapy or radiation
- It can help detect early signs of ovarian mass or ovarian cancer risk
- Some doctors also monitor granulosa cell tumors with this hormone
This keeps long-term reproductive health in check, especially after intense treatment.
7. Estimating Menopause Timing (With Limitations)
While not exact, AMH can give a rough idea of when the ovaries may slow down or stop working. This is useful in planning around possible early menopause or family building timelines.
- When AMH drops quickly, it may suggest menopause is closer than expected
- It also helps understand the risk of ovarian aging or low ovarian reserve
- Not exact, but better than waiting for symptoms
Doctors use it as a guide, along with age, cycle history, and other signs.
How the Anti Mullerian Hormone Test Works: What to Expect During Testing
The anti mullerian hormone test is a simple and painless hormone test done through a standard blood sample. It doesn't require fasting, and it can be taken on any day of your menstrual cycle, unlike some other reproductive hormones that change throughout the month.
Once the blood is drawn, the lab checks for the amount of AMH in your blood, usually measured in ng/ml. This hormone is made by small sacs in your ovaries called follicles, which hold your eggs. These values help doctors understand your reproductive hormones and overall ovarian activity.
What Happens During the Test:
- A nurse or technician collects a blood sample, usually from your arm.
- The sample is sent to a lab where the AMH level is measured.
- Results are typically available in a few days and interpreted by a fertility doctor or a specialist in clinical endocrinology.
This test is often used to check for normal AMH levels, especially when planning pregnancy, egg freezing, or IVF.
Why AMH Matters — Biologically
AMH has a special role in how we develop before birth. In female fetuses, it helps guide how the ovaries begin forming, while in males, it stops the development of müllerian ducts — the part that becomes the uterus and fallopian tubes in females.
That’s why AMH is also called müllerian inhibiting hormone or müllerian inhibiting factor. It plays a key part in sexual differentiation and can even help diagnose certain conditions like ambiguous genitalia, where the baby’s reproductive anatomy is unclear at birth.
In rare cases, AMH testing is also used to detect testicular tissue in people with disorders of sex development. This shows how widely AMH plays a role — not just in fertility, but in basic reproductive biology.
What the Test Doesn't Do
While the test gives helpful insight, it’s not perfect. It doesn’t measure egg quality, and having normal levels doesn’t always mean you're fertile. AMH is just one piece of the puzzle, used alongside other reproductive hormones and tests when doctors look at your fertility picture.
In some rare cases, issues like pelvic scarring or undiagnosed conditions can still affect fertility even if AMH looks fine. That’s why it's important to interpret results in the full context of your health.
Have questions about your AMH test or what it means? Visit DrAnshuAgarwal and get reliable guidance.
Interpreting Your AMH Test Results: What’s Normal, Low, or High

Once you get your AMH results, the next question is — what do these numbers mean? Let’s break down what’s considered normal, low, or high, and what each range could mean for your fertility.
The Risks of Ignoring Low or High AMH Levels
Some people assume AMH results don’t matter — but ignoring them can lead to delays or wrong choices in fertility planning.
Low AMH could be a sign of premature ovarian failure or early menopause. If caught early, doctors can suggest steps to protect fertility. High AMH levels, on the other hand, may point to conditions like PCOS, which can affect ovulation and treatment response.
- Low AMH doesn’t always mean infertility, but it may lower success chances in IVF
- High AMH can lead to overstimulation in fertility treatments
- Unchecked AMH levels can delay starting the right infertility treatment
AMH is not a guarantee — but it’s a warning signal that should not be skipped.
Don’t rely only on your AMH report — get real guidance from a trusted specialist: DrAnshuAgarwal
What to Do If Your Anti Müllerian Hormone Is Low or High
If your AMH is low, don’t panic. The next step is to talk to a fertility doctor about your options. Many women with low AMH still get pregnant — but you may need to act sooner or consider assisted options.
If your AMH is high, your doctor may check for PCOS or adjust fertility drugs to avoid side effects. In both cases, combining AMH with other tests gives a clearer picture.
- Consider freezing eggs if your AMH is dropping and you want kids later
- Follow up with ultrasound and other hormone tests
- Stay informed — AMH is just one part of your fertility profile
Taking early steps can give you more time, more choices, and fewer regrets later.
How AMH Levels Change With Age
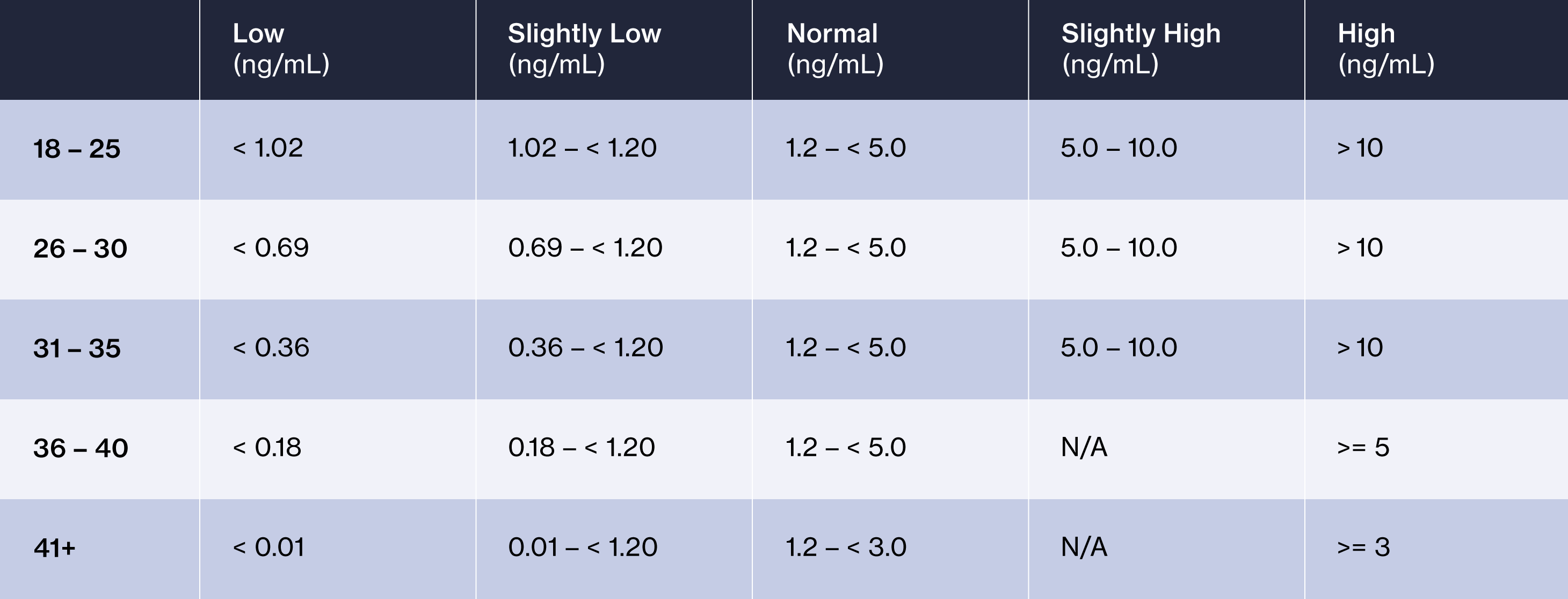
AMH doesn’t stay the same all your life. It changes with age and reflects your current egg supply.
In your 20s and early 30s, AMH is usually at its peak. As you age, your normal AMH levels slowly go down, and by the time of early menopause, they may be very low or undetectable.
- AMH starts dropping in your late 30s
- By your 40s, most women have lower AMH, even if still regular cycles
- This is a natural part of the process as your eggs decrease
Knowing this can help with planning, especially if you're thinking about delaying pregnancy or want to freeze your eggs.
7 Limitations of the AMH Test You Should Know

The AMH test is useful, but it’s not perfect. There are certain things it can’t tell you — and if you don’t know its limits, you could easily misread the results or make the wrong decisions.
1. Doesn’t Measure Egg Quality
The AMH test only shows how many eggs may be left. It says nothing about whether those eggs are healthy.
This means someone with high AMH could still have poor egg quality, while someone with low AMH might have good eggs that can lead to pregnancy.
- Egg quality drops with age, but AMH doesn’t track that
- The test doesn’t detect damage in the eggs
- Quality needs to be assessed through other methods, often during IVF
So even a “normal” result doesn’t mean your eggs are strong or ready for fertilization.
2. Cannot Predict Natural Conception or Pregnancy Success
A common mistake is thinking AMH can tell if you’ll get pregnant soon. It can’t. Many women with low AMH conceive naturally, and some with high AMH still struggle.
This is because AMH doesn’t check if the eggs can fertilize, implant, or grow into a baby.
- AMH doesn’t track ovulation or cycle timing
- It doesn’t reflect other issues like blocked fallopian tubes or sperm quality
- It’s only a small part of the full fertility picture
Use AMH to understand your reserve, not your future.
3. Not a Standalone Indicator of Fertility
Doctors never rely on just AMH. It’s always used with other tests and your health history.
A full fertility check includes hormone levels, ovulation tracking, scans, and sometimes even laparoscopy. AMH is just one number in all this.
- Always combine it with ultrasound or antral follicle count
- Other tests like FSH and estradiol help fill the gaps
- Age, lifestyle, and medical history matter more than one test result
Treat AMH as a guide — not a complete answer.
4. AMH Levels Can Fluctuate Over Time
Even though AMH is considered stable, it can still vary based on your body, stress, illness, or lab method. One test doesn’t show the full picture.
- Results may go up or down slightly across months
- Changes in health or hormones can affect levels
- Repeat testing may be needed for accuracy
This is why your doctor may suggest a second test before making big decisions.
5. Results May Vary Between Labs and Test Methods
Not all labs use the same tools or methods. That means two different labs might give different AMH results from the same blood sample.
Some tests are more sensitive than others. Also, units may differ (ng/ml vs pmol/L), causing confusion if not read correctly.
- Always check if your lab result falls in the normal range for that lab
- Don’t compare numbers blindly across sources
- Ask your doctor to interpret results using the right reference values
Where and how the test is done really matters.
6. Affected by Birth Control, BMI, and Other Factors
Things like hormonal birth control, being underweight or overweight, and other medical conditions can affect AMH levels.
For example, long-term birth control might lower the number slightly, even if your real egg count is fine.
- High BMI may also influence hormone levels
- Some medications can suppress or raise AMH
- Thyroid issues and PCOS also have an effect
These outside factors can make results tricky to interpret alone.
7. Limited Accuracy in Predicting Menopause
Some women hope AMH can tell them exactly when menopause will happen — but it can’t. It gives a clue, not a date.
Very low AMH may mean menopause is near, but it doesn’t always line up with when periods stop.
- Some women have low AMH for years and still get periods
- Others have high AMH and hit menopause early due to other issues
- It’s not a reliable tool for menopause timing on its own
Use it as a signal, not a clock.
AMH Misconceptions That Can Hurt Your Fertility Journey
Many people misunderstand what AMH really shows. These common myths can lead to poor decisions, false hope, or unnecessary worry. Let’s clear them up one by one — so you can use your results the right way.
1. High AMH Means Guaranteed Fertility
A high AMH level means you may have more eggs, but it doesn’t say anything about how good those eggs are. Fertility is not just about numbers.
Some women with high AMH still struggle to get pregnant, especially if egg quality is low or other issues are present.
- AMH doesn’t measure egg quality
- Other factors like age, sperm health, and uterus health still matter
- High AMH is sometimes linked to PCOS, which can cause irregular cycles
So even with a high number, pregnancy isn’t guaranteed.
2. Low AMH Means You Can’t Get Pregnant
Low AMH means fewer eggs, but it doesn’t mean no eggs at all. Many women with low AMH have had successful pregnancies, even naturally.
It’s a warning sign, not a final answer. It just means you may need to act sooner or look at options.
- Low AMH doesn’t mean infertility
- Age and overall health still count
- Doctors can still help with natural or assisted options
Don’t lose hope — just take informed action.
3. AMH Alone Can Predict Your Fertility Window
Some people think that AMH can tell them exactly how long they have left to get pregnant. It can’t. It gives a general idea of egg reserve — not a timeline.
- It can’t predict the exact year you’ll hit menopause
- It doesn’t measure monthly fertility
- It should always be used with other hormone levels and tests
Fertility is complex. One number can’t tell the full story.
4. AMH Reflects Hormonal Balance or Menstrual Health
AMH is not a sign of overall hormone balance. You can have normal cycles and still have low AMH, or have high AMH with irregular periods.
- AMH is not affected much by the menstrual cycle
- It doesn’t show estrogen, progesterone, or thyroid levels
- It should not be used to check for hormonal balance
For a full hormone check, you’ll need other blood tests.
5. AMH Results Are Always Accurate and Reliable
AMH is helpful — but not perfect. Levels can vary based on the lab, the test used, and even your health at the time of the test.
- Some labs use different methods with different reference ranges
- Stress, illness, or weight changes may shift AMH slightly
- A one-time test may not show long-term patterns
Always talk to a doctor to understand your results in context.
6. Over-the-Counter AMH Tests Provide Enough Insight
There are now at-home AMH tests, but they don’t offer the full picture. They can give you a number — but not the guidance that comes with it.
- These kits often skip other important tests
- They don’t check antral follicle count or egg quality
- You may misread the result without expert help
Use them only as a starting point, not a final decision-maker.
7. You Don’t Need Other Fertility Tests if You Know Your AMH
AMH is only one part of fertility. It doesn’t check for blockages, ovulation issues, male factor, or hormonal problems.
- Other key tests: FSH, LH, thyroid panel, ultrasound
- For couples, sperm analysis is just as important
- AMH alone won’t find out why pregnancy hasn’t happened
Think of AMH as a helpful tool — not a full report card. You'll still sometimes have to go for other fertility treatments
Conclusion
You've made it this far — which means you're someone who wants clarity, not confusion, when it comes to your fertility.
The truth is, understanding your body takes more than a quick search or a single test. It takes curiosity, honesty, and the courage to ask hard questions — and you're already doing that.
Whatever path you choose next, let it be one led by knowledge, not fear. You don’t need all the answers today. But knowing what to ask, and when, can change everything.
Before you take your next step, expert advice can make all the difference — see how DrAnshuAgarwal

.jpg)
.jpg)

.jpg)


